Stress tests of the cervical spine show increased pressure on the spine in the upright position. They also include flexion (looking up) and extension views. The stress on the discs can be minimal when a patient is lying down for traditional supine MRI exams. They may only show a slight disc bump or nothing at all – but no pain.
If the table is tilted vertically the bodyweight compresses the disc, causing the central disc material (or herniate) to protrude or herniate. This pinches the spinal cord and causes pain. Looking down (in flexion), puts more pressure on discs and can increase size of herniation or spinal cord compression. Patients often report feeling more pain in their fingertips or numbness. Many times, disc herniation or compression are not documented on supine images. MRIs that were taken in weight-bearing and flexion/extension will show the source of the patient’s discomfort.
Doctors can use a Stress Test MRI to diagnose and evaluate positional symptoms. Patients may feel relief if they are lying down. However, the pain, numbness, or weakness that patients experience when they move into an upright or heavier position will increase. Diagnostic, weight-bearing imaging can reveal pinched or injured nerves. This may help to explain a patient’s symptoms. Conventional supine MRIs are prone to miss 30% of spinal injuries. Get a Stress Test MRI if your pain is worse when you’re standing than sitting. You are responsible for your MRI – don’t lie down!
Overview
A herniated disc is when the gel-like middle of a spine disc ruptures through an area in the tough outer walls. It’s similar to how jelly doughnuts fill with their filling. If the disc material touches a spinal neuron, it may cause neck pain, arm pain, numbness, or tingling. Recovery begins with treatment that includes rest, pain medication, spinal injections and physical therapy. Most people recover within 6 weeks and can return to normal activities. Surgery may be an option if the symptoms do not improve.
Anatomy and Function of Discs
Your spine is composed of 24 moving bones called vertebrae. The cervical (neck)section of the spine supports approximately 10 pounds of your head and allows you to turn 180 degrees. The 7 cervical vertebrae range from C1 to C7. The discs act as shock absorbers and prevent vertebrae from rubbing together. The annulus, which is the outer ring on the disc, is also known. It has fibrous bands which attach between each vertebra’s body. The nucleus is a central gel-filled area in every disc. Each disc has a nucleus, which is a gel-filled center. Your spinal cord acts as a telephone, allowing messages (or impulses) to travel back and forth from your brain to control sensations and movement.
What is a herniated cervical spine?
A herniated disc is when the gel-like middle of your disc ruptures due to a tear in the disc wall. The gel material can be irritating to your spinal cords and cause chemical irritation. The herniated disc pressure causes nerve inflammation and swelling. You may feel partial or total pain relief as the herniation shrinks over time. In most cases, neck or arm pain will disappear within six weeks. Normal disc and herniated. The nucleus material is a gel-filled substance that escapes through the disc annulus. It then compresses the spinal cord.
There are many terms that can be used to describe a herniated disc. A bulging disc, also known as protrusion, is when the disc annulus does not break down but forms an outer layer that presses against the nerves. A true herniated disc (also called caimgfluidd, or slipped disc) is when the disc annulus cracks and ruptures, allowing for the gel-filled centre to leak out. Sometimes the herniation becomes so severe that a single fragment breaks free of the disc.
What are the symptoms of these herniated cervical spine?
A herniated disc can cause symptoms that vary depending on the exact location and your response to pain. You may feel pain radiating down your arm or into your hand if you have a herniated disc. Also, you may feel pain around your shoulder blade and neck pain when turning your neck or turning your head. You may experience muscle spasms, which is when your muscles tighten up uncontrollably. Sometimes you may feel tingling or numbness in your arm. Your triceps, biceps, or handgrip may also be affected.
Without any trauma, you may feel pain your first time you wake up. Patients who suffer from nerve pain may find relief by placing their arm behind the head.
What are the causes?
Discs can burst or herniate from injury, improper lifting, or simply by accident. Aging is a key factor. As you age, your discs can become less elastic and more dry. The tough, fibrous disc’s outer wall can become less strong. The disc wall can become weaker and the gel-like nucleus could bulge out or crack, causing pain when it touches nerves. Early disc degeneration is caused by smoking, genetics, and other occupational and recreational activities.
Who is the victim?
Most herniated discs occur in the 30s and 40s. But, middle-aged and older people are at greater risk of developing them if they are involved in strenuous activity. About 8% of herniated cervical discs are found in the neck.
How does a diagnosis get made?
Your family doctor should be consulted if you experience any pain. Your doctor will review your medical history and examine any injuries or other conditions that might be causing the pain. A physical exam will be performed next to determine the source of pain and for testing for muscle weakness.
One or more of the following imaging tests may be ordered by your physician:
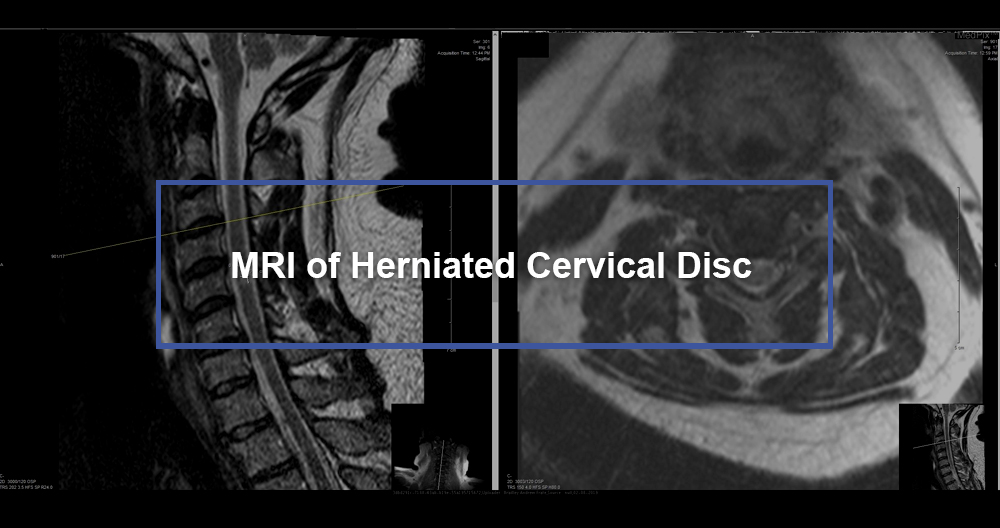
Magnetic Resonance Imaging scan (MRI) is a noninvasive test. It uses a radiofrequency wave and a magnetic field to provide a detailed view on the soft tissues in your spine. The MRI scan is clearer than an Xray. It also shows the nerves and discs. You may need to inject a dye into your bloodstream. An MRI can determine which disc is affected and if there are nerve compressions. It can detect spinal cord tumors, bony overgrowth and abscesses.
Myelogram refers to a specialized form of X-ray, where dye is injected directly into the spinal canal via a spinal tap. An Xray fluoroscopy records the images created by the dye. The myelogram’s dye will show up as white on an X-ray. This allows the physician to examine the spinal cord and canal. Myelograms can reveal nerve damage from a herniated disc or bony overgrowth. This test might be followed by a CT scan.
A CT scan (Computerized Tomography) is a noninvasive test. It uses an X-ray beam to take 2D images of your spine. The dye (contrast agent), may be injected into your bloodstream. This test is particularly useful in confirming the disc’s condition.
EMG and NCS: These tests measure electrical activity in the nerves and muscles. A special machine records the results from small needles (or electrodes) that are inserted into your muscles. The nerve is unable to supply movement and feeling to the affected muscle because of the pressure caused by a herniated disc. These tests can detect nerve weakness and damage.
X-rays can be used to view your bony vertebrae and tell your doctor if you have any arthritic conditions, bone spurs or fractures. This test is not sufficient to diagnose a herniated or bulging disc.
Diagnostics for Cervical Radiculopathy Using a Herniated Disc
A herniated disc can lead to cervical radiculopathy. This diagnosis is usually made after a thorough medical history is taken and a physical exam. A doctor may conduct one or more diagnostic tests to confirm the diagnosis of cervical radiculopathy. This involves having the patient bend their head to the side that is painful and then seeing if gentle pressure can create or temporarily trigger symptoms.
Advanced diagnostics can be requested if additional information is needed in order to confirm the diagnosis. An MRI scan is the most common option. This uses a strong magnetic field to image the cervical spine. The scan will show if a disc has been displaced onto a nerve. An alternative option to imaging the cervical spine is CT scan with myelogram. This allows for the visualization of soft tissue and can be done if the patient is unable for an MRI.
What treatment options are there?
Nonsurgical conservative treatment is the first step towards recovery. It may include medication, rest and physical therapy. Home exercises, hydrotherapy and chiropractic care are all options. In six weeks, 95% of those suffering from arm pain caused by a herniated spine experience improvement and return to normal activities. If conservative treatment fails to work or the symptoms persist, your doctor might recommend surgery.
Non-surgical Treatments
- Self care: Most herniated disc pain will disappear within a few days. In the majority of cases, it will go away completely in four to six weeks. Restraint in activity, heat therapy, and over-the-counter medication will all help with your recovery
- Medication: Your doctor could prescribe pain relief, nonsteroidal-anti-inflammatory medication (NSAIDs), or steroids. Sometimes, muscle relaxers can be prescribed to treat muscle spasms.
- Nonsteroidal anti-inflammatory drug (NSAIDs), such as aspirin, naproxen (“Aleve, Naprosyn”), ibuprofen (“Motrin Nuprin, Advil), celecoxib (“Celebrex”), are some examples of nonsteroidal, anti-inflammatory medications that can be used to reduce inflammation or pain.
- Although analgesics such as Tylenol (acetaminophen) may relieve some pain, they don’t have the same anti-inflammatory effects as NSAIDs. Long-term consumption of analgesics or NSAIDs could cause stomach ulcers.
- Muscle relaxants like methocarbamol (Robaxin), soma (Soma), and carisoprodol/Soma (Soma), can be used to treat muscle spasms.
- The nerve swelling and inflammation may be reduced by steroids. They can be taken orally as a Medrol dose pack in a tapering amount over a five-day span. It can provide pain relief in as little as 24 hours.
- Steroid injections are performed using x-ray fluoroscopy. The procedure involves the injection of steroids and a numbing agent in the epidural space. To reduce swelling and inflammation of nerves, the medication is given directly to the affected area. The epidural injection will provide relief to approximately half of the patients. However, these effects tend to be temporary. You may need to repeat the injections in order to get the full effect. Pain relief may last from weeks to years. Injections may be combined with home exercises and/or physical therapy.
- Physical therapy: Your goal in physical therapy is to get you back to full activity as quickly as possible and to prevent injury from happening again. Physical therapists can help you improve your posture, lift, and walk, and will also work with you to strengthen, stretch, and stabilize your neck, shoulder, arm, and back muscles. They will encourage you to stretch out your spine and strengthen your arms. Your treatment should include strengthening and exercise.
- Holistic therapies include acupuncture, acupressure and yoga.
Surgical Treatments
If symptoms don’t resolve or progress with conservative treatment, surgery may become an option. When planning surgery, factors like patient age, length of problem, previous neck operations, and expected outcome will all be considered.
An anterior approach to cervical disc surgery (front of the neck) is the best. A posterior (from behind) approach can be used if there are other conditions like stenosis or need for cervical disc surgery.
- Anterior cervical discectomy & Fusion (ACDF). The surgeon makes a small incision at the front of your neck. To expose the disc and bony vertebrae, all neck muscles, nerves, vessels and nerves will be removed. The disc portion that has ruptured is taken out. To create a fusion, the space between the disc and nerve may be filled with bone or cage grafts. Fusion is the joining of more than one bone. Over time, the graft will fuse with the vertebrae below and above to form one solid bone. For stability during fusion, and possibly to improve the rate of fusion, screws and metal plates may be used.
- Artificial disc replacement: An anterior discectomy involves inserting a device that imitates the natural motion of a disc into the damaged joint space. Fusion does not eliminate motion. An artificial disc preserves movement. These artificial discs are made from metal and plastic. They look like hip and knee joint implants. However, the outcomes of artificial disc surgery compared to ACDF (the standard), are similar. Cervical disc replacement preserves motion and possibly avoids adjacent-level disease. This hypothesis has yet to be proven.
- Minimally invasive microendoscopic discectomy: A small incision is made in the back to remove the disc. For enlarging the tunnel to the vertebrae, small tubes known as dilators can be used. The nerve root and disc are exposed by removing a portion of the bone. To remove the damaged disc, the surgeon will use an endoscope or microscope. This technique is less painful than traditional discectomy.
- Posterior cervical discectomy. The surgeon makes an incision about 1-2 inches in your back. The spine muscles are cut to expose the damaged disc. To reach the nerve root space and disc space, we need to remove a portion of the bony arch. Carefully remove the part of the ruptured disc that has been causing compression to the spinal nerve. In order to prevent future pinching, the spaces through which nerve roots exit the spine are usually enlarged.
Clinical trials
Clinical trials involve the testing of new treatments, including diagnostics, procedures and therapies on patients to verify their safety and effectiveness. The standard of medical care is constantly improving. The Internet contains information on current clinical trials including protocol details, eligibility, and location. You can also sponsor studies through the National Institutes of Health and private industry.
Recovery and Prevention
8/10 people suffer from back pain at one time or another in their lifetime. It usually disappears after 6 weeks. Recovering from back pain requires a positive attitude, regular exercise, and a quick return to work. It is in the best interests of patients to return to modified (lighter or restricted) duties if their regular job is not possible. For short periods, your doctor can prescribe such activity.
Preventing recurrences is key.
- Proper lifting techniques
- Good posture when standing, sitting, moving, or sleeping
- An appropriate exercise program can be used to strengthen weak abdominal muscles, prevent re-injury and keep you fit.
- An ergonomic work space
- Healthy weight and lean mass
- Stress management and a positive attitude are key to a successful life.
- No smoking
