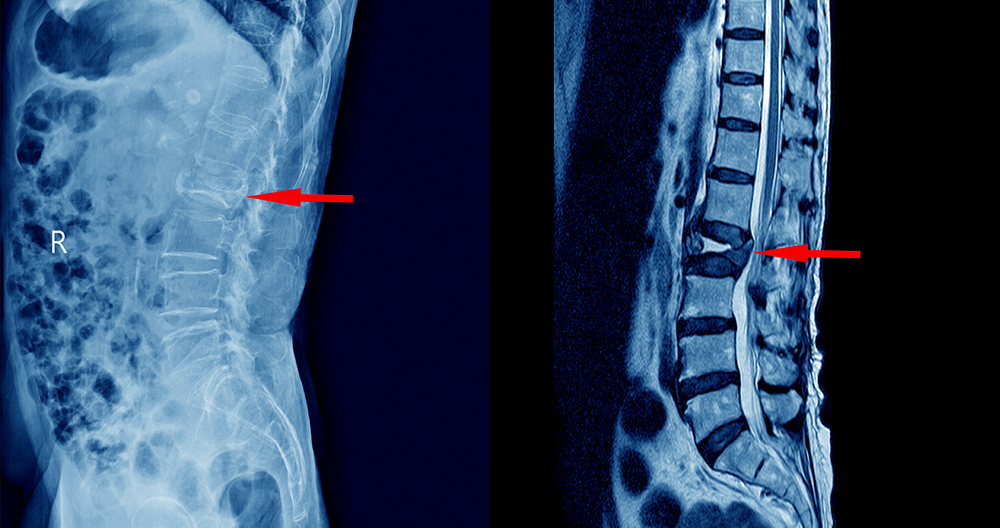
MRI scans are used frequently to diagnose and monitor herniated spines. They can be used in a variety of ways, including to locate the herniated disc(s), and determine the level of nerve compression. Your doctor might recommend additional tests to help diagnose a herniated or bulging disc. MRIs are helpful in diagnosing bulging discs in neck and back and herniated discs.
What your Doctor might Do
Once your doctor has ordered your MRI, the technician will place you inside a tube-shaped device. The device rotates a magnetic field around the patient, changing the amount of excitation of hydrogen atoms within the tissues. Once the magnetic field is removed the hydrogen atoms are in their normal resonance and release a small amount of energy. This energy can be detected by the scanner to produce the image, known as the MRI scanning.
The generated MRI scan image shows anatomy. This is done by distinguishing between tissues that contain a lot (such cerebrospinal fluid, discs, or other fluids) and tissues that contain very little water (such skin, bone and cartilage, as well as nerve roots). Your doctor will review the image and diagnose any anomalies. MRI scans are sensitive to detect disc injuries, such as a bulging disc or bulging disc.
How to read an MRI for a Herniated Disc
There are several factors that influence the interpretation of an MRI scan. Similar to many other diagnostic tests such as MRI scans, the challenge with MRI scan results is that the “disorder”, which is shown on the MRI scanner, does not always indicate the cause of backaches.
Patients must have a basic understanding of how lumbar MRI scans are done to determine if there is a herniated or damaged disc. These discs are usually in constant motion which can cause wear and tear. The annular tear occurs when the disc’s outer shell is damaged. This causes the inner nucleus jelly to leak into the spinal canal and form a hernia. This hernia is often visible as a contrast spot in an MRI.
The physiological symptoms that the patient experiences and exhibits in MRI scans are what will interpret the results. An herniated disc may not present symptoms on its own. However, there are many people who suffer from undiagnosed back conditions. The herniated disc can cause severe pain if it becomes bulged or protrudes. This video explains how disc herniations can lead to back pain.
Back pain occurs when the herniated disc becomes inflamed along its posterior annular tear. The pain signals travel via the sinuvertebral nerve located along the margin of the annulus fibrosus. The somatic afferent pain fibers located along the posterior annulus fibrosus wall are called the primary sensory cortex. They project pain signals to the region of the brain where there is highly localized pain.
Herniated disc causes
There are 23 intervertebral Discs located in the spine. These discs are tissue joints which protect the spinal vertebral bodies from any unexpected impact. They have an inner soft gel-like and an outer firm wall (annulus fibrosus). An annular tear is a crack in the disc’s outer wall that allows the jelly-like nucleus of the disc to pass through. If there is little nucleus justify in the annular tear this is known as a bulging or herniated disc.
Many reasons can lead to a herniated disc. The most common cause of a herniated disc is injury or wear and tear. As we age, the cartilage that connects the discs in our spine to the vertebral members can become looser. Herniated discs can also occur from sudden trauma and impact such as falls or injuries.
Symptoms of a herniated disc
Herniated discs can cause irritation of nearby nerves. The annular tear develops when the nucleus pulposus interacts with the smaller blood vessels located in the outer 1/2. An area of inflammation in the disc’s back is where a particular type of pain neuro fiber is present. The pain signals travel via somatic sensory nerves (SA), to areas of the brain that are responsible for localizing the pain. The somatic afferent(SA) fibers end-up synapsing to neurons within the postcentral gyrus. This area is also known as the primary sensory cortex. This part of the brain provides pain signals from the body with their location tag, as well as associated qualities like “sharpness”, “stabbing” and “sharpness”. The posterior annulus is the only area that is innervated with SA pain fibers. This allows us to easily distinguish disc pain location from disc quality. Click here to watch animation
Sharp pain is the most common sign of a herniated or inflamed disc. The disc herniation inflammation can cause nerve irritation and even headaches by spreading to the spinal cord and dural cover. Cervicogenic headaches refer to neck pains that radiate upwards from the back of your skull. Permanent headaches disappear when the disc is properly repaired using the Laser Disc Repair method.
Inflammation from the herniated disc spreads to the surrounding nerve roots. Pain sensations can travel down the arms (cervical herniation), legs (lumbar herniation), or around the ribs and thoracic herniation. Nerve root dermatome is the most obvious area to notice signs and symptoms of a herniated spine. The nerve root dermatome is the most common area to notice loss of normal sensation in your arms, elbows, and shoulders. Cervical Radiculopathy, the medical term for this condition, is marked by radicular discomfort in the area and the appearance of a hot sensation radiating outside the source of the pain.
Disc herniation can cause disc herniation to the nerve root myotome. This refers to the muscles of the arm and leg that are controlled by the nerve root. This causes weakness in the muscles of this area, including the triceps. It may be difficult for patients to move these anatomical parts.
Four Best Treatment Options for a Herniated Disc
Below are some of the most effective surgical treatments for herniated discs.
Spinal Fusion Surgery / Spinal Arthrodesis
During any spinal fusion surgery, the surgeon permanently unites or fused more than one vertebrae. Although the vertebrae fuse to create one solid, long bone, all natural movement is lost forever. This procedure is designed to mimic the natural healing of fractured bones.
Bone grafts may be taken from the patient’s own hip, taken from a cadaver bone or made ahead of time. For fusion to take place, bone grafting and metal implants are required. Over 100 patients who had bone grafts were diagnosed with Tuberculosis after receiving the bone grafts. This unfortunate event highlighted the serious complications that can result from invasive spinal surgery like artificial discs or spinal fusion.
Spinal fusion is performed by a surgeon. They remove the disc, place a bone-graft between the painsome and painful vertebrae, and fuse the vertebrae together to create a unit. Although the pain is limited, the solid unit causes permanent movement loss. Common complications can lead to severe and even fatal problems.
There are many variations of Spinal Arthrodesis.
- Anterior Cervical Discectomy and Fusion
- Posterior Cervical Decompression and Fusion
- Transforaminal Lumbar Interbody Fusion TLIF
- Extreme Lateral Interbody Fusion
- Anterior Lumbar Interbody Fusion – ALIF
Discectomy Surgery
A discectomy is a procedure that removes an external herniated disc. This relieves nerve root pressure. It doesn’t treat neck pain or back pain. However, it can relieve arm or leg pain. The surgeon enters the patient’s spine and makes holes in the bones and ligaments to reach the herniation. The surgeon uses a variety of tools to cut through the tissues surrounding the vertebra. He then removes bone, ligament, and eventually the entire herniated portion of the disc. The amount of herniation a surgeon can remove is limited by the amount they are able to see. Since it is impossible for them to see all of the herniation during a discectomy they only manage to remove the most significant.
A discectomy refers to “cutting out the disc.” Patients can have one disc or several removed at one time. Different vertebrae are called “levels.” To perform a discectomy, the surgeon uses an “open” approach. A surgeon may make a larger incision than for minimally invasive procedures to view the spine.
Because of the difficulty in seeing and the tools used during surgery, discectomy surgery is highly susceptible to nerve damage and infection. This technique is older and doesn’t use microsurgery, or the endoscope.
Microdiscectomy Surgery
The microdiscectomy is very similar in appearance to a discectomy. The procedure uses a microscope with a 2-3 inch incision. A microdiscectomy involves the surgical removal of disc material and placing pressure on nearby nerve roots. During the procedure, the surgeon will make a 2-3 inch incision across the back of the patient above the ruptured disc. Next, the surgeon removes bone and ligaments of the spine in order to access the hernia. After cutting away the muscle, the surgeon then cuts the muscle. This procedure is used to treat sciatica, which is a condition caused by compression of spinal nerves. This procedure is not effective in relieving back pain. It can make the problem worse. Microdiscectomy is a procedure that allows patients to return to their normal activities within a few years. Many people who undergo microdiscectomy also have to undergo additional surgeries to repair the damage done by the original microdiscectomy.
Laser Disc Repair is not an option for surgeons who are not able to treat leg weakness and numbness caused by a herniated or bulging disc. Stability is common because the surgeon must cut through normal spine bones, ligaments, joints, and other structures to reach the herniated dis. Many patients will need to have a second or third procedure to repair the damage done to the first. Because the microscope is used, this surgery is more likely to be performed at an infected hospital. Microdiscectomy involves the surgeon inflicting minor injuries on the patient’s muscles and bones to remove the herniated disc. Additionally, because of the high number of complications, the surgeon will need to prescribe highly addictive opioid painkillers to help with recovery. Additional surgeries are likely to be needed.
Artificial Disc
Patients who have tried all sorts of pain medications and physical therapy, but still suffer from unrelenting leg or arm pain may be candidates for artificial disc replacement. The surgeon replaces the damaged disc with an implant made of plastic or engineered metal during artificial disc surgery.
The disc is replaced with an artificial one that functions similarly to a natural. Surgeons reach the spine by removing delicate organs from the abdomen or neck. Many surgeons and patients avoid the anterior (through your belly) surgery to fix lumbar disc issues. This procedure is dangerous because of the serious complications that can be caused by it.
Patients are advised to plan to remain at the hospital for a minimum of two days following an artificial disc replacement. In most cases, they will be able to return home within a few days. Within 24 hours, most patients can walk again. The goal of fusion is not to remove pain, but to preserve motion at the affected disc.
What’s the average time it takes for a herniated disc to heal without surgery?
Herniated discs often heal naturally. These cases can heal in as little as two days, or even less than four weeks. Most herniated disc cases do not require surgery. These cases can be treated with simple treatments, such as resting for a couple of days and making small lifestyle changes for a few months to ease the symptoms. Patients often notice symptoms disappearing within weeks, or even days. If symptoms or pain from a herniated/bulging disc lasts longer than 4 weeks, the Laser Disc repair should be performed. The body’s other muscles and joint will begin to deteriorate, causing further pain and dysfunction. Patients should not wait longer than 2 to 3 months after symptoms appear. It can lead to more pain and complications, which in turn will reduce the quality of your life.
You may be able to relieve a herniated disc by performing a variety of exercises. These exercises can be performed by anyone regardless of fitness history or previous experience. Low-impact exercises are recommended as they offer the most pain relief and discomfort while working on certain muscle groups.
Slipped disc The Importance Of MRI To Detect a Herniated Disc
A herniated disc, also known by the slipped disc or the degenerated disc, is a common condition. It occurs when a damaged disc becomes displaced due to injury, old age, or degeneration. In this situation, the disc’s soft cartilage is pulled out of its outer shell. Herniated discs can sometimes be invisible, but severe pain can occur if the exact location is not obvious. A slipped disc usually heals itself, although it is possible to have therapy or surgery.
How is a Herniated Disc diagnosed?
A consultant Healthcare Professional will not recommend an MRI if a patient has any of these symptoms. Usually, a MRI scan is not required if chronic pain does not resolve after 6 weeks of conservative treatment, including stretching exercises, massages, pain relievers, and pain relief medication.
Many patients with herniated discs in the neck and lower back recover well after non-surgical treatments. Some patients may need to have a more comprehensive examination or imaging to confirm.
Imaging tests are used to confirm the presence or absence of a herniated disc. This is especially important when surgery is necessary. To check for a herniated disc in the neck, or in any other part of the spine, a CT scan or MRI scan may also be ordered.
MRI, among all imaging options, can provide the most accurate snapshot of the spine and aid in diagnosing a herniated disc. An MRI scan is able to pinpoint the exact location of the herniated disc and can also help in measuring the extent of the herniation.
An MRI scan may also be helpful in improving the accuracy of surgeries and the time taken to recover.
Unusual pain on the spine is worth a visit to a physician in any case. Early diagnosis and treatment can be initiated if a bulging, or ruptured disc is found. This reduces the chance of developing irreversible complications.
A number of factors are important to consider when undergoing an MRI. These include limitations in interpretation and timing of the scan.
Evaluating MRI Scans Results
The problem with MRI scans as with other diagnostic studies is the possibility that the “abnormality,” which may be seen on the MRI, might not be the actual cause of the back pain. Numerous clinical studies show that about 30% of those in their thirties to forties have a lumbar Disc Herniation, even though they do not experience any back pain.
A MRI scan cannot be interpreted alone. All information on an MRI must be correlated to the individual patient’s circumstances, including:
- Symptoms (such pain’s duration, location, severity and duration)
- Any neurological problems that were discovered during their physical examination
A key consideration when MRI scans will be performed is the timing. A patient with either of these conditions will require an MRI scan immediately.
- Incontinence in the bladder and bowel
- Nerve damage causes progressive weakness in the legs.
Fortunately, neither of the above scenarios are common.
Commonly Asked Questions
Can an MRI be used to diagnose a herniated disc?
Some physicians still recommend CT scanning or X-rays. Herniated disc MRI is still the best diagnostic procedure, as it provides the most accurate imaging for the condition and does away with unnecessary radiation.
However, MRI scanning may be delayed by clinicians if there are persistent and worsening symptoms. A combination of conservative treatment interventions may be used to ease the pain and improve the patient’s condition. Although most people are able to recover without any major surgery, some may require additional treatment. This is when MRIs are often prescribed.
Is a herniated disc the same as a ruptured disc?
A herniated or ruptured disc is the same spinal condition. It will show more protrusions than a bulging disc. Scans will also reveal that the cartilage usually held within the spine is leaking out to the outer, more rigid cartilage. Because it is likely to press on nerves it causes more severe pain than a bulging disc.
What happens to a herniated disc if it is not treated?
A herniated disc can worsen if it isn’t treated immediately. Most cases of slipped disc can be managed without the need to have surgery. A non-surgical treatment for a herniated disc can include relaxation, physical therapy and the use of painkillers.
Neglecting to treat the condition can result in permanent nerve damage. This condition can cause loss of bladder control and bowel control. It can also lead to sensation loss around the thighs or rectum.
Can MRI detect herniated discs?
A MRI scan is used to confirm a herniated-disc diagnosis. It can pinpoint the area of the spine showing herniation. This allows for better management of treatment, which may in some cases involve surgery.
What causes herniated disc?
Multiple causes can lead to a herniated disc. disc herniation can also be caused by accidents and normal wear and tear due to aging. These are just a few of the possible causes.
- Poor posture
- Unnecessary strain on your back is often caused by lifting heavy objects, especially if they are in an unsuitable position.
- Overweight or obese can place unnecessary pressure on the spine.
- Regular physical activity is not enough