Treatments for conditions that affect the L5-S1 spine motion segment are often nonsurgical. Surgery may be required if lower back or leg symptoms persist or become worse despite nonsurgical treatments.
What is L5 S1 Fusion Surgery and how can it help you?
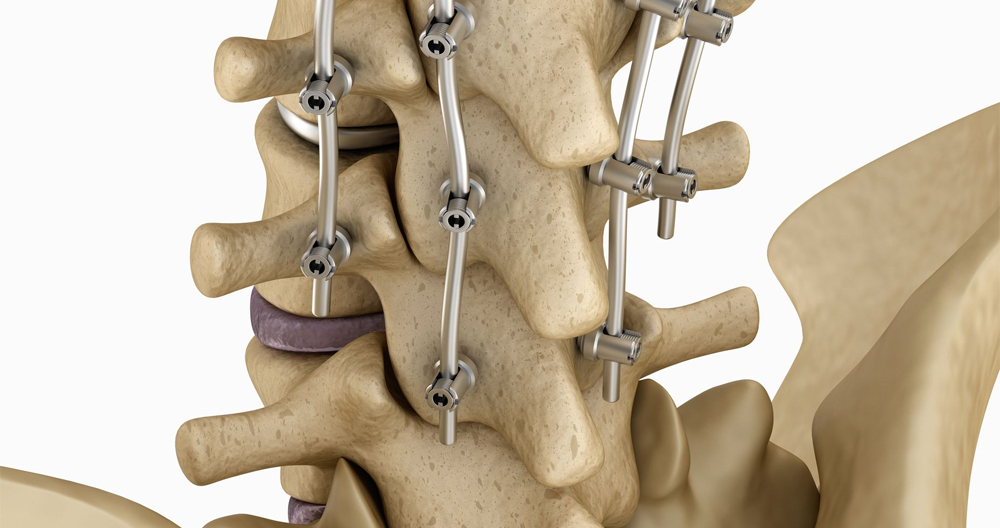
Spinal fusion refers to major surgery in which one or more of the spinal bones (vertebrae), are fused using screws, bolts and/or plates. The hardware can either be located in the anterior (posterior), or posterior (posterior). Often, the disc between spinal bones is removed and replaced with bone. L5 Fusion is the level of surgery.
Five spinal bones are located in the lower back. They are numbered L1, 2, 3, 4, and 5. Between each of the spinal bones is a disc. The name of the disc comes from the two spinal bones it’s sandwiched between. The L5/S1 disc is the lowest disc at the low back. The L5/S1 is sandwiched between L5 and the S1 spinal bones. L5 S1 surgery is the procedure to remove the L5/S1 disc and fuse the L5 and S1 spine bones together. There are many options for surgical procedures. A case in point is posterior lumbar interbody (PLIF), which has been described in detail in a previous blog.
What are the signs of L5-S1 Fusion?
Lumbar fusion is a well-known surgery. In the United States, lumbar fusion has grown in popularity from 77,682 surgeries to 210,407. Lumbar fusion can treat many degenerative conditions and pains in the low back. L5 S1 fusion is used for the following conditions: Low back disc problems (spondylolisthesis), Spinal Bone Fracture, Recurrent Disc Herniation, Curvature (Scoliosis), Narrowing of Canal (Stenosis), Failed Spine Surgery.
Is Spinal Fusion Major Surgery Possible?
Absolutely! This surgery involves cutting through important muscles and ligaments to reach the targeted disc. The disc is then removed. The area is then packed with bone, and sometimes a spacer. Stabilizing the spine is done by placing screws into the spinal bones. Additional hardware such as rods and plates are used to support the screws.
What is the Success Rate for Spinal Fusion Surgery Surgery?
As it relates spinal fusion surgery success is not easy to determine. Why? Because of the many variables involved, such as the preoperative MRI, surgical approach and x ray finding, results from pressing on the disc, patient’s ages, medical history, and the parameters that were studied.
Take the following example: After fusion surgery, 53 patients were surveyed for 20 months. Patients with normal MRIs had only 50% improvement after surgery. 40% of patients dissatisfied/uncertain about their outcomes 2 years after lumbar spine fusion reported ongoing back pain, and limited daily function. Another study showed that the failure rate of lumbar spinal surgery was between 10% and 46%. These statistics will show success rates for l5 s1 procedures.
Spinal Fusion Can Screws Come Loose?
Yes! Yes. There are many complications that can arise from L5-S1 fusion. Failed fusion is where the bones don’t properly fuse.
Non-Union
Non-union refers to the failure of spinal bones bolted together to fuse or grow together. Rates will vary depending on which type of lumbar spinal fusion procedure is being performed. The rates of non-union for procedures that require more bone (e.g. posterior fusion) can be as high at 26-36%
Broken Screws in Lumbar Fusion
Lumbar fusion involves using screws, bolts and plates to stabilize the spine bones. Hardware and the low back are subjected to significant forces. These forces can lead to spinal instability and pain. One study found that hardware failure occurred at an alarming 36%. Sometimes additional surgery is required to repair or replace hardware that has failed.
Hardware is loosening up
Lumbar Fusion uses screws to stabilize your spine. The same forces which can cause hardware to crack can also cause screws to loosen. This can cause spinal instability and even pain. A third of patients who have had a low-back fusion will need to have another surgery to correct nonunion or hardware failure.
Additional Complications after L5 S1 Fusion Lumbar Fusion
As a result of lumbar Fusion, there are many problems. Adjacent Segment Disease, and Spinal Muscle Injuries are two of the most serious.
Diseases of the adjacent segment
The disc is an important shock absorber. Fusion surgery removes the important shock absorber and places additional stress and pressures on the discs, facet joints and other structures above and below the level. This can result in disc and facet joint injury, which can lead to arthritis and degeneration. This is a problem that affects 9% of people. This can cause additional surgeries such as fusions.
Spinal Muscle Injury
The spinal muscles are critical for supporting the spine and providing stability. Lumbar fusion is a serious risk to the integrity and health of these muscles. This can result in spine instability and other injuries, such as arthritis and degeneration. VA is a recent client who was treated in our clinic for this issue. VA was suffering from severe low back pain and underwent lumbar surgery several years ago. Unfortunately, the pain didn’t improve even after the surgery. This is his low back MRI. It shows the death of the vital low back muscles. The MRI image is a cross section. The yellow arrows indicate dark, healthy spine muscles. The left side shows the results of the surgery. The yellow arrows signify the muscles that were damaged and are now dead from fusion surgery.
What is lumbar discectomy and how does it work?
Discectomy literally translates to “cutting out a disc.” A discectomy is performed anywhere along the spine. It can be done from the cervical area (neck) to low back (lumbar). The surgeon accesses the injured disc from the posterior part of the spine, through the muscles and bone. The surgeon will remove a small portion of the lamina from the disc. The lamina forms the backside to the spinal canal and covers the spinal cord. Next, the spinal cord is pulled to one side. Depending upon your case, you may need to remove one disc (single level) or multiple (multi-level).
A discectomy can be performed using a variety of surgical techniques and tools. The “open” method uses large skin incisions and muscle retractions to allow surgeons direct access to the area. A “minimally invasive” or microendoscopic discectomy requires a very small incision. The tubes are progressively larger and called dilators. They tunnel through the muscle. Special instruments are used to allow surgeons to see and operate in a smaller amount of space. A minimally invasive procedure may be less disruptive to the back muscles and reduce recovery time. Your surgeon will determine the best option for you.
For patients with spinal instability, athletes, heavy laborers, or those who perform heavy lifting, fusion can be performed simultaneously with discectomy. Fusion involves using a combination of bone glue and hardware (screws/plates), in order to connect two vertebrae. During healing, the vertebrae fuse to form one piece of bone. A herniated lumbar disc is rarely required for fusion.
Who is a candidate for the job?
If you have any of the following symptoms, you may be a candidate to have a discectomy.
- Myelogram, CT, MRI and CT are diagnostic tests that can detect a herniated disc.
- Significant pain, weakness or numbness in your foot or leg
- Leg pain (sciatica), is worse than backache
- Physical therapy and medication have not helped with symptoms
- Cauda Equina syndrome is characterized by leg weakness, loss feeling in the genital areas, and loss control of bladder or bowels.
For leg pain due to:
- Bulging or herniated disc: This gel-like material can burst through a weak spot in the wall surrounding the disc (annulus). When this material squeezes out and painlessly presses against a nerve, it can cause irritation or swelling (Fig. 1).
- Degenerative disc Disease: The discs naturally begin to wear, and bone spurs are formed. Inflamed facet joints. The discs become brittle and lose their cushioning and flexibility. The disc space gets smaller. These changes can cause disc herniation and stenosis.
The surgical decision
Most herniated discs heal within a few months of nonsurgical treatment. Although your doctor might recommend certain treatment options for you, you will have to decide if surgery is the right choice. Before you make a decision, be sure to weigh all the pros and cons. After six weeks of nonsurgical treatment, only 10% of herniated disc patients feel sufficient pain to warrant surgery.
Who does the procedure?
Spine surgery is possible by an orthopedic surgeon or a neurosurgeon. Many spine surgeons specialize in complex spine surgery. Ask your spine surgeon about their training, particularly if you have had more than one surgery.
What happens prior to surgery?
The doctor will ask you to sign consent and other forms. This allows the surgeon to learn about your medical history (allergies/vitamins/bleeding, allergies, anesthesia reactions and previous surgeries). Your doctor will discuss all medication (prescription, over the counter, and herbal supplements) with you. Presurgical tests, such as blood test, electrocardiogram and chest Xray, may be required several days before your surgery. Check with your primary physician to determine if you can stop using certain medications or if you are ready for surgery.
Keep taking the prescribed medications as directed by your surgeon. Non-steroidal antiinflammatory medicines such as naproxen, ibuprofen, and others should be discontinued. and blood thinners (Coumadin, aspirin, Plavix, etc.). 7 days before surgery. Avoid bleeding and problems caused by alcohol and nicotine use at least one week before and two weeks following surgery.
Before surgery, you might be asked to wash your face with Hibiclens (CHG), or Dial soap. It kills germs and reduces the risk of infection at the surgical site. It prevents CHG from entering the eyes, ears, nose, or genital area.
Morning of surgery
- You should not eat or drink after midnight, unless you have been told otherwise by your hospital. With a small glass of water, you may be allowed to take certain medicines.
- Use an antibacterial soap for showering. Wash loose, clean clothes.
- Wear flat-heeled sneakers with closed backs.
- Remove make-up, hairpins, contacts, body piercings, nail polish, etc.
- You can leave all jewelry and valuables at home.
- Take a list with all medications and their dosages, as well as the times they are usually taken.
- Take a list with you of all allergies to medicines and food.
- You should arrive at the hospital approximately 2 hours before your scheduled surgery (surgery center about 1 hour prior). This will allow you to complete any paperwork or pre-procedure work ups. An anesthesiologist can talk to you about the benefits and risks of anesthesia.
What happens during surgery?
The procedure is broken down into five steps. The entire operation takes approximately 1 to 2 hours.
Step 1: Prepare the patient
After being anesthetized, you will lie on your back on a table. You will be able to lie down on your stomach, with your chest and sides supported. Preparation is required for the incision to be made.
Step 2: Make an Incision
The fluoroscope is a special X-ray that allows the surgeon to pass a thin needle through skin until the bone. This helps to locate the affected vertebrae and disc.
Open discectomy is a procedure that involves cutting the skin down to the middle of your back and removing the affected vertebrae. The number of discectomy to be performed will affect the length and depth of the incision. A single-level incision measures approximately 1 to 2 inches. The bony vertebra is exposed by the muscles of the back. A X-ray scan is taken to confirm that the correct vertebra has been identified.
An open discectomy requires a 1-to 2-inch skin incision (blackline) at the middle of your spine. Retraction is done to the one-side of muscles overlying the vertebrae. A small, non-invasive discectomy is performed by inserting a small needle (green line) into the skin at the midline.
A discectomy is minimally invasive and involves a very small incision on one side of the back. To gradually separate the muscles, a series progressively larger dilaters are passed around one another to create a tunnel leading to the bony vertex.
The muscles are gradually dilapidated with increasing size tubular retractors for minimally invasive discectomy.
Step 3: Perform a laminotomy
Next, a small cut is made in the lamina. This will be done above and below your spinal nerve. A laminotomy may be performed on either one side (unilateral), both (bilateral), or multiple vertebrae. A laminotomy creates a small window by removing bone from the top and bottom of the lamina. You can gently reflect the nerve root or spinal cord to expose herniated discs
Step 4: Discard the fragments
The surgeon removes the lamina and gently retracts the protective cap of the nerve root. The surgeon examines the disc through a surgical microscope. To relieve the pressure on the spinal nerve root, only the disc that has ruptured is removed. The entire disc cannot be removed. Also, any bone spurs or synovial cysts that might press on the nerve roots are removed.
The nerve root is being removed from the compression of the herniated disc material. Fusion is only performed when there is a single level of lumbar discectomy. Other conditions, like recurrent disc herniation and spinal instability, can be treated with fusion.
Step 5: Close the incision
The retractor which holds the muscles in place is taken out. The skin and muscle incisions will be joined with staples or sutures. The incision is sealed with skin glue.
What happens following surgery?
The postoperative recovery area will allow you to wake up. Monitoring will be done to monitor blood pressure, heart beat, and respiration. Any pain will also be treated. After you are awakened, you can start gentle movement, such as sitting up, or walking. Most patients can return home within 24 hours. In a matter of days, other patients can be discharged from the hospital. For the first 24 to 48 hour, make sure you have someone to support you at home.
Follow the surgeon’s instructions at home for two weeks after surgery or up to your follow-up appointment. In general, you can expect:
Restrictions
- Avoid twisting and bending your back.
- You shouldn’t lift any object that is more than 5 lbs.
- You are not allowed to do any strenuous activity, such as housework or yard work.
- You shouldn’t drive within the first two to three days of taking pain medicine or muscle relaxers. If you have pain under control, you may be able to drive.
- Don’t drink alcohol. It reduces blood flow and can cause bleeding. It is important to not mix alcohol with pain medication.
Incision Care
- Showering the day after surgery is possible if Dermabond glue is applied to your incision. Use soap and water to gently clean the incision every day. Do not rub the glue. Pat dry.
- Stitches, steri strips, and staples may be removed by you showering 2 days following surgery. Every day, wash the area gently with soap and warm water. Pat dry.
- You can cover drainage with a gauze dressing. Call the office if drainage is able to penetrate two or more dressings within a day.
- You should not take the incision into a swimming pool or bathtub.
- Apply no lotion or ointment to incisions.
- After every shower, wear clean clothes. Make sure to use clean sheets and linens when you go to bed. Keep pets out of the bed until your incision heals.
- Your follow-up appointment will remove any stitches, steri strips, or staples.
Medications
- As directed by your surgeon, take pain medications as prescribed. Your pain will subside and you will be able to reduce the dosage and frequency of your medication. You don’t have to take pain medication.
- Constipation can result from using drugs like Narcotics. Get lots of water, and eat high-fiber meals. To help your bowels move, stool softeners and laxatives may be useful. Over-the-counter alternatives include Senokot, Dulcolax, Miralax, and Colace.
Activity
- For 15-20 minutes, you can ice the incision three to four times a day to reduce swelling and pain.
- If you are asleep, don’t lie down or sit in one position for more than an entire hour. Stiffness can cause more pain.
- Walk for 5-10 mins every 3-4 hours. Gradually increase your walking as you become more fit.
When should you call your doctor
- Fever greater than 101.5deg (unrelieved using Tylenol).
- Unrelieved nausea or vomiting.
- Incision infection symptoms
- Itching and rash around the incisions (allergy Dermabond Skin glue).
- Tenderness and swelling of the one-leg calf.
- New symptoms of weakness or tingling in the arms or legs.
- Excessive sleepiness, dizziness, confusion, nausea, or dizziness.
Recovery and Prevention
Your surgeon should schedule a follow-up appointment for two weeks after your surgery. For some, physical therapy may be required. The length of recovery depends on the extent of your health issues and the type of disease. There may be some discomfort at the incision site. It is possible that the original pain will not disappear completely after surgery. Try to maintain a positive attitude, and follow the instructions for physical therapy.
For jobs that don’t require physical challenges, most people can return work in less than 2 to 4 week. Some jobs, such as those that require heavy lifting or the use of heavy machinery, may take up to 8 to 12 weeks for others to return to work.
Back pain recurrences are quite common. Preventing recurrences is key to avoiding them.
- Proper lifting techniques
- Good posture when standing, sitting, moving, or sleeping
- Appropriate exercise program
- An ergonomic work space
- Healthy weight and lean mass
- Relaxation techniques, such as stress management, can be aided by a positive attitude.
- No smoking
What are the results?
A good result is achieved in 80-90 percent of patients who undergo lumbar discectomy. Results from a study comparing nonsurgical and surgical treatment of herniated discs were:
- People suffering from leg pain (sciatica), are more likely to have surgery than people with back pain.
- Nonsurgical treatment works well for those suffering from less severe or increasing pain.
- People who have suffered from moderate to severe pain and had surgery see a greater improvement than people who did not.
- Minimally invasive discectomy has been shown to have comparable outcomes to open discectomy. Although minimally invasive techniques offer a shorter operating time, less blood losses and muscle trauma, as well as faster recovery times, these newer techniques might not be suitable for all patients. Ask your surgeon if microendoscopic discectomy, which is minimally invasive, is right for you.
The discectomy may offer faster pain relief than other surgical treatments. It isn’t clear whether surgery will make a difference in the type of treatment that may be required. A recurrent disc herniation is a condition in which 5 to 15% of patients have it on the same or opposite side.
What are the possible risks?
Surgery is not without risk. The most common complications of any surgery are bleeding, infection, blood clots and reactions to anesthesia. The risk of complications is greater if spinal surgery is performed at the same time. The following are some complications that may arise from a discectomy:
Deep vein thrombosis is when blood clots build up in the veins. The risk of lung collapse and even death exists if the clots become detached and travel to your lungs. There are many options to stop or treat DVT. To prevent your blood from clotting, get up as soon as you can. The blood can be kept from pooling in the veins by wearing a support hose and pulsatile socks. Coumadin and Heparin are also possible.
Lung problems. After surgery, the lung must be functioning at its best to ensure that tissues have enough oxygen to heal. A collapsed lungs can result in pneumonia. Your nurse will tell you to breathe deeply and to cough frequently.
Nerve damage and persistent pain. Every operation on the spine can cause damage to the nerves or the spinal cord. The nerves and spinal cord can be damaged, which could lead to paralysis or numbness. Nerve damage due to a disc herniation is the main cause of persistent, severe pain. Sometimes disc herniations can cause permanent nerve damage, rendering it unresponsive for decompressive surgery. In such cases, spinal cord stimulation and other treatments might provide relief. Make realistic expectations about your pain before you go to surgery. Your doctor will discuss your expectations.
Nonsurgical Treatments of L5-S1
Treatment for L5-S1 often begins with:
- Medication. Pain stemming from L5 to S1 are best treated with an over-the-counter (OTC), medication, such as nonsteroidal antiinflammatory drugs (NSAIDs). For severe pain, prescription medications, such as opioids and tramadol, may be considered.
- Physical therapy. You can target pain from L5 to S1 with specific exercises or physical therapy. These therapies can help stabilize the back and keep your muscles and joints strong for long-term relief. They also provide healing for lower back tissues.
- Chiropractic manipulation. The manipulation of the lumbar spine by chiropractic adjustment might help relieve pain that stems from L5 to S1.
- Self-care. Heat and ice can be used at home to treat mild to moderate pain. For sciatica, it is best to remain active and carry out daily activities as tolerated. Bed rest may temporarily alleviate symptoms but it does not usually lead to a faster or longer-term recovery of sciatica.
- An exercise program, quitting smoking and losing weight can all help to lower the risk of complications from L5/S1.
Injection Treatments for L5-S1
After nonsurgical pain relief methods have been tried for several weeks, and before surgery is considered, injections could be considered.
The most common L5-S1 injection treatments are:
- Lumbar epidural steroid injections. The spinal epidural space is a place where steroids can be injected directly. They are able to reduce inflammation and the sensitivity of nerve fibers to pain. These injections work better for pain caused by inflammatory factors, such as pain from fragments of herniated discs. They are less effective for pain that is compressive.
- Radiofrequency ablation. Radiofrequency ablation is a treatment for pain that stems from the L5-S1 facet joints. A radiofrequency needle is used to heat a part of the pain-transmitting neuron in order to form a heat leak. This causes the nerve to stop sending pain signals back to the brain.
- Fluoroscopic (x ray-based) guidance is used to ensure correct needle placement when performing injection treatments. Fluoroscopic guidance with contrast dye helps improve diagnostic accuracy and reduce procedural risk.
As a diagnostic tool, injections may also be used as a selective nerve block to confirm the root cause of leg pain.
Surgical Treatments for the L5-S1 Region
If neurological deficits such as numbness or weakness persist after several weeks of nonsurgical treatments have been exhausted, surgery may be considered. If a structural condition is not responsive to nonsurgical treatment, surgery is recommended. There are several procedures that can be done to relieve nerve root compression and/or cauda horsemena.
- Microdiscectomy is the procedure where a small amount of disc material is removed near the nerve roots. The nerve root can also be cut to relieve pressure.
- Laminectomy is the removal of a part or all the lamina (area bone behind the vertebrae), in order to make room for the cauda Equina.
- Foraminotomy (intervertebral foramen), is an operation to expand the opening for the spine nerve root (intervertebral canal foramen). It relieves pressure by trimming bony excess.
- Facetectomy is the removal of nerve roots from the facet joint.
- Lumbar interbody fusion: Degenerated discs are removed, and the L5-S1 vertebrae fused together using implants or bone grafts. When performing a spinal fusion, the risk of failure (pseudarthrosis), in fixing the S1 segment is usually higher than for L5. An interbody support, which holds the vertebrae together, is often recommended to avoid this problem.
A surgeon may perform multiple procedures at once. A laminoforaminotomy (also known as a laminectomy and foraminotomy) is a combination of a laminectomy and a foraminotomy. Open surgeries are possible in certain instances, though these procedures can be done minimally invasively.
Patients who don’t have progressive neurological changes might not respond to non-surgical care. Some patients may not be candidates for surgery because of other medical conditions or drug addiction.
Spine surgery can lead to infection, nerve injury and excessive bleeding. Discuss the risks and options with your surgeon before you make a decision to have surgery. It is important to know what complications may occur if the surgery is not performed.
Conclusion
L5 S1 Fusion is major surgery in which the L5/S1 disc and L5 and S1 spine bones are removed. L5-S1 fusion is for severe pain and dysfunction caused by degenerative disc disease. The parameters that were examined can affect the success rate. Patient satisfaction is low. There are many complications, including non-union failure, hardware breaking or hardware becoming loose. Fusion surgery can also cause injury of the spinal muscles or adjacent segment disease. These complications can be avoided if fusion surgery is not performed in the first instance.