Intervertebral Discs are found between the vertebrae on the front end of the spine. They act as shock absorbers. The two main components of a disc can be compared to a jelly-doughnut. The annulus, which is the outer portion of the disc, is composed of fibrous tissue rings that look like tires. The nucleus, which is the inner part of the disc, is also known as the annulus. The nucleus, which is composed of protein molecules, attracts fluid that acts as a shock absorber and cushion between the vertebrae.
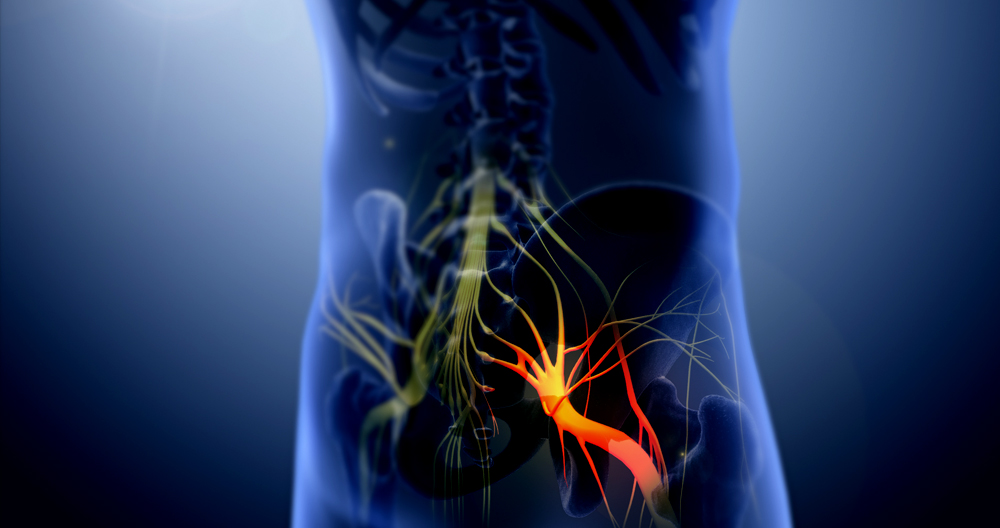
Disc herniation refers to the process whereby some nucleus material, which is located in the middle of the disc, has moved out of it through a tear or crack in its outer annulus. Most often, the defect in an annulus is located at the back. The nucleus material can squirt into the spinal channel where it can irritate or compress a nerve root. This results in sciatica which means that you have leg pain. Sciatica is severe leg pain. Many people say it is worse than childbirth or kidney stones. Most people suffering from disc herniations feel severe leg pain. Most cases of disc herniation are not caused by any specific injury. It can occur in anyone, regardless of their size or occupation. The most common age group is between 20-49. Some people feel back pain that lasts for a while before they start feeling the leg pain. This could be due to the tear in their outer disc.
The disc herniation determines the nerve root affected and how it affects leg pain distribution. The 2nd and 4th lumbar vertebrae are where disc herniations are most common. Both can lead to pain running from the buttock down to the calf and foot. Some people experience numbness in their foot or leg, while others experience weakness in their leg. The good news is that between eighty and ninety percent of people can recover without the need for any treatment. Most people recover in three to six months. Ten to twenty percent don’t recover fully.
The pain can sometimes be relieved by physiotherapy and chiropractic manipulation. No matter what type of treatment, disc herniation pain will improve gradually in most people. This is the “natural history” of the condition. Some people have disc herniations that completely disappear. Others don’t experience any pain. According to studies, the cause of the pain may be due to the release of inflammatory chemicals. These chemicals help to dissolve the disc and also irritate nerves. When this inflammation is over, the pain disappears. Stretching the leg, for example, can cause nerve irritation and further aggravate pain. While it is important to be active, avoid activities that can aggravate the pain. Many activities, such as swimming, walking, or cycling, can be done without aggravating pain. It is possible to remain active without causing nerve damage. Nerve damage occurs in less that 10% of disc herniations. This can lead to weakness or numbness in your leg. The majority of cases, nerve damage occurs right after the disc herniation. It is rare for nerve damage to occur later.
The pressure on the nerve can be relieved by surgery to remove the herniated fragment of disc. This can relieve leg pain almost immediately in between eighty and ninety percent. There are risks associated with surgery, such as infection and injury to the nerve. Surgery is rarely an option. But complications are rare in less than one percent of surgeries. About one in 100 will suffer permanent nerve damage from disc herniation. This can lead to weakness, numbness, and even permanent pain.
Because of the severe pain, people who have suffered a sciatica episode are often afraid to resume their normal activities. Recurrent disc herniation is possible after the symptoms have resolved. It is estimated that 10% of people will experience this again. Recurrence can occur regardless of whether the patient had surgery. It can happen quickly or many years later. Most people recover completely from disc herniation. They can return to work or other activities. Regular core strengthening exercises can help prevent disc herniation and the onset of back pain.
Sciatica vs Herniated Disc
My fellow clinicians have faced a whole new set of problems in the age of the internet. The greatest problem is patient self-diagnosis.
The internet is an enormous information resource. Information about everything is available online, including information about Ancient Rome and Elon Musk’s latest venture. This doesn’t mean you have to believe everything you read here is true.
Even if all the information is accurate, it doesn’t mean you are correct in your diagnosis. You are not a physician, at least most of those who read this aren’t. To arrive at these diagnoses, doctors and therapists use complex diagnostic tools. These tools can’t be found online, so it’s impossible to diagnose yourself from WebMD.
This was the first thing I did before answering the question: “What’s the difference between sciatica & a herniated spine?” I have had patients tell me that they believed they had one or another based upon what they had read online. There are many subtle differences in the debate about sciatica vs herniated disc.
I’ve received everything from blank stares and tears to my face when I had to explain to them that their diagnosis wasn’t correct. Sciatica and herniated disc can both be linked, but the conditions are completely different. Let’s look at sciatica vs. herniated discs.
Sciatica
The largest nerve in your body is the sciatic. Five nerve roots are located in the sciatic nerve. The sciatic nerve runs from the back of each leg and can cause pain, burning, tingling, difficulty walking, and discomfort while seated. The pain can extend as far as the feet.
Herniated Disc
These cushion-like components protect your vertebrae. They’re filled with a liquid-like fluid. The fluid pushes out of the disc’s hard casing, causing nerve pressure and pain.
The difference
The difference between sciatica and herniated discs is that sciatica can usually be treated within a short time. Herniated discs require more attention. These are chronic conditions. The impact on quality life and quality of your daily activities is even more serious if left untreated.
The two conditions could easily be confused at the outset. It is difficult to determine which condition is present without the diagnostic tools we mentioned earlier. Sometimes, an MRI is necessary to clearly see all physical systems involved in order for clinicians to make an accurate diagnosis. A herniated disc can sometimes cause sciatica. But the opposite is not true. These are the major differences between sciatica or a herniated disc.
Selective Nerve Root Blocks
What are selective nerve root blocks? A selective nerve roots block is a spinal procedure that uses anesthetic to place anesthesia on a particular nerve root of the spine. This helps identify the exact cause of leg pain. This test can be used for a diagnosis when it is necessary to determine the optimal level for injections or surgical intervention. The injection often contains painkillers and inflammation to lessen the pain. This injection is very similar to a transforaminal steroid injection. However, in a selective root block, there is no attempt to inject the medication into the epidural space. Instead, the goal is to completely cover the nerve root.
How are epidural steroid injections and selective nerve root blocking performed?
The fluoroscopic X Ray is used to place the patient on their stomach. Before the injections are performed, it is important to thoroughly clean the skin with an antiseptic. The skin is first numbed with local painkillers. A small spinal needle is then inserted using fluoroscopic guidance into the correct position in the spine.
For epidural steroids injections, and selective nerve root blocks, the final needle position should be just above the target root. For an epidural steroid injection using the caudal approach, the needle is passed through a tiny opening (sacral Canal) just above the tailbone. An epidural steroid injection is performed using an interlaminar approach. The needle is passed between two vertebrae. To verify proper needle position, contrast dye is injected.
The medication will then be injected. The procedure takes approximately 15 to 30 minutes and involves close monitoring of vital signs. For continued monitoring, the patient is transferred to the post-procedure region.
What is really injected?
The injection typically consists of a mix of a local and steroidal anesthetic (e.g. Marcaine(r), Lidocaine)
Is the process painful?
Most of the time. Patients say it is as painful and uncomfortable as a routine blood exam.
What should I expect following the procedure?
Anesthetic can be placed around a nerve root and epidural space to cause temporary numbness. The steroid medication could begin working as soon as 6 hours or 3 days after injection. Some people may experience some soreness up to 2 days after receiving the injection. This period may be helped by ice. In one to five working days, you might start to feel significant pain relief.
What should I do after the procedure?
After the procedure, it is a good idea to have someone drive your home. Patients should rest and reduce their activity for the first day. You can apply ice to any soreness around the injection site.
What is the best time to get back to work?
After the procedure, you can continue with your daily activities as long as it is not painful.
How many injections do I need?
We rarely perform more than three injections per 12-month. The likelihood of side effects could increase if the injections are performed more frequently.
Are there any potential risks?
This procedure is considered very safe. As with all procedures, there are risks as well as possible side effects.
The following complications can be caused by epidural steroid injection or selective nerve root blocks:
- Common: Pain at the injection site
- Infrequent worsening symptoms
- Infection – rare
- Bleeding – rare
- Very rare – severe spinal cord or nerve injury
The steroid medication may also cause side effects such as:
- Fluid retention – uncommon
- Weight gain is rare
- Elevated blood pressure is rare
- Rare mood swings
- Insomnia is rare
Suppression of the body’s natural cortisone-producing ability – rare
What if I am taking Coumadin®, another blood thinner?
No. No. It is possible that you will be asked to temporarily suspend your blood-thinning medications, but this should not be done without consulting your doctor.
Who should not get an epidural or selective nerve root block?
If you are:
- You are at risk of excessive bleeding if you take anticoagulant (blood thinning) medication.
- The cause of your back pain is an infection or malignancy.
- You have a local or systemic bacterial infection.