Just below the belt line is the L5-S1 segment of the spinal column. It is the final segment of the lower spine, which articulates with the tailbone (sacrum). According to published studies, 80% of adults will experience back discomfort at some point in their lives. Back pain is most commonly caused by disorders of the L3-L4, the L4-L5, or the L5-S1 lumbar segments. Back pain is most commonly linked to the L4-L5 or L5-S1 segments.
The Spine can be divided into five sections:
- There are seven vertebrae total in the cervical spine (neck).
- Twelve vertebrae make up the thoracic spine (upper, middle-back).
- Five vertebrae make up the Lumbar spine (lower back).
- Sacrum is a triangular bone which articulates with both the L5 and L5 pelvises to form the tailbone. The coccyx, a triangular-shaped structure located at the base of the spine’s tip, is small.
INTRODUCTION
Low back pain (LBP), one of the most common conditions, is herniated disc lumbar. LBP is also one of the most prevalent problems. Lumbar discectomy has been a common procedure for neurosurgeons for decades. Cauda equina syndrome, also known as lumbar disc herniation, is a serious neurologic disorder. Radiculopathy and back pain are two of the most common symptoms. You may experience urinary retention that causes incontinence and/or rectal dysfunction. It is important to suspect saddle anesthesia. However, the pathophysiological mechanisms of CES are still not fully understood.
It could be caused by direct mechanical compression of Cauda Equina nerve roots (CE). This is a common problem that can lead to disability at work. It is rare to find sexual or sphincter dysfunction due to a prolapsed lumbar intervertebral disc. This has not been well investigated. This study aims to determine the possible mechanisms and outcomes of sexual and sphincter dysfunction caused by lumbar disc herniation.
The L5-S1 Spinal Segment and Back Pain
The lower lumbar spine can be injured and worn. A host of conditions and diseases that can affect the lumbar spine can interfere with your daily activities.
These are some symptoms and conditions that can be associated with L5-S1 spinal section disorder.
- Pain in the back, buttocks or legs
- Tingling, burning, or numb sensations in the feet, buttocks, legs, feet or toes
- Walking difficulties or inability to stand for short periods
- Paralysis in either one or both of the legs
- Bowel and balder disorders
- Infertility, impotence and sexual dysfunction are all possible.
What is the Best L5-S1 Treatment?
It is best to treat spine disorders conservatively, such as those that are related to L3–L4, L4–L5, or L5–S1. The last resort should be to have more invasive procedures, such as RFA (radiofrequency ablation) or steroid injections.
Radiofrequency ablation, also known as RF ablation, is a minimally invasive spine surgery procedure that kills the pain-sensing nerves in your spine. This treatment can cause degenerative changes in your spine, which is caused by nerve damage and soft tissue injury. We advise against it.
Focused conservative treatments are required to treat back pain caused by L3-L4,L4-L5,L5-S1, or L5-S1. These treatments fix or repair any injured or damaged areas. Combining physiotherapy and chiropractic is the best way to treat back pain. Common areas of pain and disability are the lower lumbar segments (L3–S1) Common causes of leg and back pain are degenerative discs, arthritis (bone Spurs), and slip discs.
L5-S1 Spinal Segment Problems that Cause Back Pain and Leg Symptoms
Patients suffering from back pain often have problems with the L5-S1 segment of their spine. The following conditions can cause back pain caused by the L5-S1 spinal segment:
- Muscle spasms : Sometimes, this is the first sign that you have back pain.
- Joint problems (spinal joints misalignment, arthritis or degeneration) are common. Neglecting a spinal issue can lead to more serious problems such as bone spurs and facet hypertrophy.
- Pinched nerves: This is caused by slipped discs and bone spurs. It can also be caused by ligament thickening, as in Ligamentum Flavum hypertrophy and facet hypertrophy.
- L5-S1 spondylolisthesis: L5-S1 spondylolisthesis refers to a condition where the 5th segment of the lumbar (L5) slides forward relative to the 1st sacral segment (S1). Spondylolisthesis is most common at the L5-S1 segment. The most common site for spondylolisthesis in the L5-S1 segment is the L5-S1. A L5-S1 Spondylolisthesis may be congenital or developmental.
- Degenerative changes: The most common cause of back pain is degenerated spinal discs, spine joints or soft tissues. Degeneration of your spine discs, soft tissue degeneration, or degeneration could all be the causes of back pain.
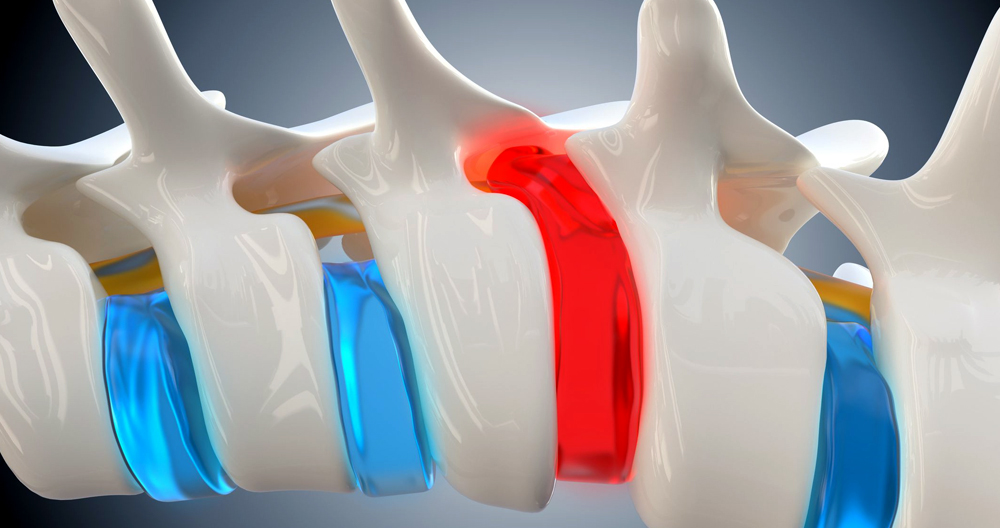
- Slipped disc: This is the layman’s term for bulging discs or herniated discs.
- Sciatica is a group or bundle of nerves that originate from the exiting spinal nerves L4-S3. Sciatica and sciatic-like pain syndromes are mediated by the L5-S1 segment.
- L5-S1 Spondylosis: Excessive weight bearing or repeated injuries due to spondylosis, or arthritic degradation of the vertebral body margins and spinal discs at L5–S1 can lead to spondylosis.
- Posterior Facet Hypertrophy L5-S1: This medical term refers to the spinal joints. Each segment is made up of four facets. The connection of the facets below the vertebrae to the facets above creates spinal joints. Back pain is often caused by facet hypertrophy.
- Spinal canal Stenosis at L5-S1: The spinal canal is the tunnel or passageway for the spinal cord and spinal nerves after the cord ends. The spinal cord terminates at L1 and descends as nerve fibers, which resemble horse tail hairs. The most common causes of shrinkage or stenosis of the spinal canal are spondylosis, hypertrophy of Ligamentum Flavum, slipped discs and spondylolisthesis.
- Hypertrophy of Ligamentum Flavum L5-S1 : Ligamentum Flavum, an essential ligament, is responsible for connecting spine bones and providing stability during movement. It’s especially important when bending or extending. Any segment can experience Thickening or Hypertrophy of Ligamentum Flavum. Hypertrophy or thinning of Ligamentum Flavum at the L5-S1 segment is less common than it is in L3-L4 or L4-L5 segments.
- L5-S1 Foraminal Stenosis: These are the openings through which nerves exit from the spine. Nerve impingement can be caused by shrinkage in the foramen (hole). Foraminal stenosis (vertebral foraminal stasis) is common in the slipped disc, spondylolisthesis and hypertrophy Ligamentum Flavum.
Expert care is required to diagnose and treat an L5-S1 condition. These are the steps you should take to improve your back pain treatment.
Back pain caused by L5-S1 problems
Back pain is most commonly caused by the L4-L5 or L5-S1 segments. Problems arising from L5-S1 are mainly due to xial loading (weight-bearing activity). Long-term sitting or standing puts enormous strain on the L5-S1 disc and spinal joint. Excessive weight bearing and prolonged sitting for long periods of time can cause disc pressure to increase (increased intradiscal pressure).
The intradiscal pressure is measured using mm Hg (millimeters mercury). Healthy intradiscal pressure should be below 70 mmHg. Blood flow will decrease if the intradiscal pressure is higher than 70 mm Hg. In addition, an increase in intradiscal pressure can cause a decrease in blood flow and impede the absorption of nutrients and other compounds that are necessary for maintaining a healthy spinal disc.
The body’s position and daily activities directly affect the intradiscal pressure (spinal disc pressure). Here are some examples of intradiscal pressures in different positions:
- Supine position: The average intradiscal pressure in this position is 25 mm Hg
- Standing straight: The intradiscal pressure rises to 100+ mmHg
- Standing while bending at the waist: Intradiscal pressure rises up to 150+ mm Hg
- When sitting properly and upright: The average intradiscal pressure of 200 mm Hg
- Poor postures can lead to intradiscal pressure of 250+ mm Hg
The most vulnerable segment of the spine is the lumbar spine (lowerback) due to the negative effects of elevated intradiscal pressures from prolonged sitting or standing.
L5-S1 Disc Bulge And Disc Herniation Causes, Signs & Symptoms
The most common site for disc bulge or disc herniation (slipped disc) is the lumbar spine. L4-L5 is the most common location for a slipped disc in the lower back. L5-S1 is the second most common area of involvement. The third most common location for herniated discs is L3-L4.
Herniated discs L5-S1 are most often caused by premature wear and tear of the spinal discs. All disc-related conditions, including disc degeneration, can cause herniated discs at L5-S1. Healthy discs won’t herniate. People with degenerated or damaged discs are more likely to develop a herniated L5/S1 disc. The following are common causes of spinal disc herniations:
- Prolong sitting
- In a forward-bending position, sit down
- Excessive twisting or bending at the back
- Improper lifting
- Slip and fall
- Injuries
A herniated L5–S1 disc can press on nerves and the spine. The compression can cause discomfort, aches and pains in the buttocks. It can also lead to tingling, numbness, and weakness in the legs, legs, knees or ankles, feet, feet, or fingers.
L5-S1 pinched nerve symptoms include stiffness, tingling, weakness, and numbness. Nerve pain can be described as a burning, sharp or throbbing sensation that radiates to the lower limbs, giving rise to sciatica-like symptoms.
Sciatica pain occurs when one or more nerves of the cervical spine are compressed or irritated. A sharp, burning feeling can be felt in the sciatica area. It starts in the lower back and moves up the leg. This affects the distribution of nerves in the feet. Sciatica pain can radiate down to the buttocks. However, its distribution will depend on which nerves are affected.
L5-S1 Spinal Segment Issues Can Cause Back Pain and Leg Symptoms
Lower back problems, such as intervertebral disc issues in the lower back, can often cause leg pain. Patients with severe neck, upper, or mid-back problems that compress the spine cord can also feel pain in their legs. Expert care and analysis is crucial in diagnosing the cause of leg pain.
A slipped disc, also known as a disc bulge or herniated disc, can press on a nerve causing pain, numbness or weakness. Compressed nerves, L4-L5/L5-S1 impingement or compression of the spinal nerves, or pain in the legs or buttocks may cause pain.
Any segment with a spinal disc can have a bulging or herniated disc. In the neck and lower back, bulging and herniated or slipped discs can be common. Slipped discs in the neck could involve the C4–C5, C5–C6, or the C6–C7 segment. Slipped discs in the lower back are more common at L3-L4, C4-L5, and L5-S1.
Sciatica-like sensations, which are pain and numbness in the back, can be caused by herniated or slipped discs. In severe cases, it can also cause pain, numbness, and difficulty urinating.
Sciatica & The Spinal Segment L5-S1
Sciatica can be described as pain in the back, hips and legs that is caused by compression of sciatic nerve fibers from the lower end to the lower extremities.
Sciatica pain occurs when the nerve fibers of the sciatica nerve become compressed in the spinal cord, Thecal Sac, or exiting the spine. Sciatica can also be caused by congenital anomalies, excessive muscle tightness in the piriformis muscles – a deep muscle located in the buttocks.
Spinal canal Stenosis is a common source of back pain
The spinal canal is the tunnel formed by interlocking segments of the spine to house the spinal chord. The spinal cord is a cylinder-shaped, rope-like bundle of nerves that starts at the base of the skull and continues downwards inside the spinal canal to the L1 or first lumbar segment. The L1-L2 spinal level is where the spinal cord transforms from a solid, rope-like cylinder into strands similar to horse’s tail (solid portion and strands). At the point where the rope-like structures become hair-like strands, or rootlets, the cord is called cauda Equina (from Latin horse’s tail).
Cauda Equina Syndrome & Back Pain
Cauda Equina syndrome is a condition that causes compression and impingement to the nerves of the thecal sac (nerves within the spinal canal). This occurs in the lower spine. Three of the most common causes for cauda-equina syndrome are slipped disc, arthritis and hypertrophy in the Ligamentum Flavum. These conditions compress the spinal cord, nerve roots, and the sac as they exit the spine canal. Cauda Equina Syndrome will affect most patients.
Cauda Equina syndrome is characterized by debilitating pain in your lower back and lower extremities. It can cause paraesthesia, weakness, difficulty walking, and in extreme cases, intestinal or bladder disorders.
A cauda-equina syndrome is characterized by debilitating pain in your back and lower extremities as well as difficulty walking in the legs and paraesthesia. Cauda Equina syndrome can also be characterized by sexual and reproductive dysfunctions as well as bowel and intestinal issues and bladder disorders.
Cauda Equina Syndrome is most commonly caused by the L4-L5 or L5-S1 segments of the spinal segment. The most common causes of cauda equina syndrome are slipped discs, thickening the posterior vertebral bodies (spondylosis and arthritis), and hypertrophy in the Ligamentum Flavum.
Anatomy and Structure of the L5-S1 Spinal Motion Section
These structures are common to this motion segment:
L5 and S1 vertebrae. There are many differences between the L5 and S1 vertebrae.
- L5 is composed of a vertebral head in front and an arch at the back. It has three bony protrusions, a prominent spinous process in its middle and two transverse processes along the sides. These protrusions are used as attachment points for ligaments.
- The sacral base or S1 is also known as the sacral top. It is the higher and wider end to the triangular-shaped sacrum. The body of S1 is composed of the top and wing-shaped bone on each side. This is called the alae. The median ridge, a bony prominence at the back of the S1 vertebra, is located at the bottom. On the left and right sides of this ridge, there are bony openings called foramina.
- The articular cartilage is used to connect L5 and S1 at their joint.
- L5-S1 intervertebral disc. Between the vertebral bodies L5 and S1, a disc is made from a gel-like material (nucleus pilosus), which is surrounded by a thick fibrous ring. This disc protects the vertebrae from shock-absorbing and cushioning effects during spinal movements.
- L5 spinal nerve. The L5 spinal nerve roots leave the spinal cord via small bony openings (intervertebral foramina), on the right and left sides of the spinal canal. These nerve roots combine with other nerves to form larger nerves that travel down each leg and extend down the spine.
- The L5 dermatome, which is a part of the foot, knee, and leg, receives sensations from the L5 spinal neuron, is an area of skin.
- The L5 myotome, a group of muscles controlled via the L5 spinal nervous system, includes certain muscles in the pelvis and legs that are responsible for foot and leg movements.
- The L5-S1 motion section provides a bony enclosure to the cauda, which are nerves that run down from the spinal chord and other delicate structures.
Common Problems at L5 – S1
The L5-S1 located at the bottom vertebral column is often subject to excessive biomechanical stresses, which can lead to higher loads and increased injury risk. These are some of the most common problems:
- Problems with the disc. Lower back disc herniation usually occurs at the L5 to S1 level. This disc’s steeper slope leads to higher shear stresses, which can lead to disc injury and degeneration.
- Facet joint pain. Facet joint pain.
- Spondylolysis. Spondylolysis is a condition that affects the L5 vertebra. It is the fracture or dislocation of the pars interarticularis, a small piece of bone at the intersection of the vertebral arches and facet joints. This can happen on either one or both sides. It is common for the bone to not break but instead become stressed. This condition is known as a pars stress reaction.
- Spondylolisthesis. The condition of spondylolisthesis is when the pars of L5 break on both sides. Most often, spondylolisthesis L5 is due to repetitive stress to the interarticularis. It is most common in children and teenagers. It is rare to see a pars fracture caused by trauma.
- Malignant tumors such as sacral chondromas, although rare, can occur at the L5-S1 levels. Other problems at this level include developmental variations in S1, fusions of L5 and S1, extra facet joints, and fusions of L5 and S1.
Common Signs and Symptoms that Stem from L5-S1
L5-S1 disc and vertebral pain can develop suddenly after an injury, or slowly over time. A dull ache or sharp pain in the lower back is common. Discogenic pain can be worsened by sitting for too long, being in one position, repetitive lifting, and bending.
Radiculopathy symptoms and sciatica can be caused by inflammation or compression of the L5 or S1 spinal nerve roots.
- Pain is generally described as a shooting, sharp, or searing sensation in the buttocks, thigh and/or feet.
- Numbness in the toes and/or foot
- A weakness in the foot and/or leg muscles, and inability to lift the feet off the ground (foot drop).
- A stabbing pain or ache can also be caused by a dermatomal area. These symptoms usually affect one leg at the time but can sometimes be felt on both legs.
Cauda Equina syndrome can occur at L5 to S1 because of injury to the cauda-equina nerves which descend from the spine. This is a medical emergency that can cause severe pain, weakness and numbness in the legs, genital area, and/or both legs. You may also experience loss of bladder and bowel control. This condition should be treated immediately to preserve leg function, and to restore bowel or bladder function.