L4-5 and L5–S1 are the most common levels for herniated discs. A sharp, burning, stabbing sensation is the sign of a herniated disc. It radiates down the leg to the below of the knee. It is typically superficial and localized in nature and can be accompanied by tingling or numbness. In some cases, motor deficits or diminished reflexes may be present in advanced cases.
A central disc herniation is a rare condition that can cause low back pain, saddle pain in the S1-S2 distributions. A central herniated spine may also cause nerve root compressions of the cauda-equina. This can lead to difficult urination or incontinence. An examination and medical history may reveal bladder or bowel dysfunction. For permanent function loss, emergency surgery is necessary in these cases.
It is often difficult to distinguish between low back strains and herniated spines when evaluating patients suffering from symptoms of a herniated central disc. The pain from low back strain is worsened by standing and twisting movements, while the central disc herniation pain is worse when a patient sits or is in a position that puts more pressure on the annular fibers. The patient may need to be asked if the pain was worse while driving to the appointment, or sitting in the waiting room. Sitting, bending and standing postures can increase the pressure on the intervertebral disc7. This explains why patients in a sitting position experience more symptoms of herniated disc.
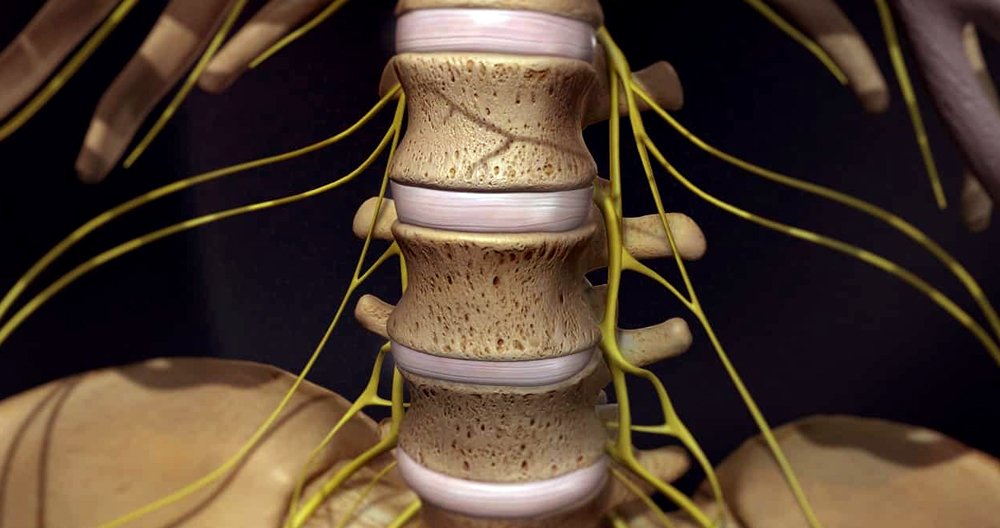
Anatomy of L5-S1 Spinal Motion Segment
The following structures are typical of this motion segment:
L5 and S1 vertebrae. Different features distinguish the L5 from S1 vertebrae.
- L5 includes a vertebral body at the front and an arched back with 3 bony protrusions. There is a prominent spinous center and two transverse processes on each side. These protrusions act as attachment points to ligaments.
- The sacral base also known as S1 is the higher and wider end of the triangularly-shaped sacrum. S1 consists of a body at the top and wing-shaped bone on either side. This is called the alae. The median ridge is a bony prominence located at the back of S1 vertebra. This ridge has bony openings (foramina), on both the right and left.
- The L5-S1 facet joints are lined with articular cartilage and join them.
- L5-S1 intervertebral disc. The disc between the vertebral bodies S5 and L5 is made of a gel-like material (nucleus pulposus). It is enclosed by a fibrous ring (annulus fibrosus). This disc acts as a shock absorber and cushion to protect the vertebrae when they move.
- L5 spinal cord. The L5 spinal neural roots exit the spinal cord through small bony foramina (intervertebral foramina), located on the left and the right sides of the spinal canal. These nerve roots are joined with other nerves and form larger nerves which travel down the spine.
- The L5 dermatome (or L5 skin area) receives sensations via the L5 spinal nerve and can include parts of the leg, foot and knee.
- An L5 myotome, a group of muscles controlled via the L5 spinal nervous, is responsible for foot and leg movement.
- The L5 – S1 motion segment provides a bony cover for the cauda equina (nerves running down from the spinal cord) and other delicate parts.
Common symptoms of a herniated spine L5/S1
- Back Pain: The most common symptom associated with a herniated L5/S1 disc is back pain. This may shock you but not everyone who has a herniated spine experiences back pain. Although it was shocking to see clients with a herniated spine but no back pain, it is possible. The most common symptoms of a herniated disc L5/S1 are aching or sharp pains in the lower back. It may feel tender to the touch or as if your muscles are spasming.
- Sciatica is caused by a herniated disc L5/S1. Sciatica is a term we use to describe the pain in the back of the leg. It is often severe and painful. Clients describe it as “being stabbed by hot poker”.
- Pins and Needles/Numbness: A herniated L5/S1 disc can cause sensory changes in the foot or leg. These sensations can occur in the foot and the toes. In some cases, they may be more painful than the pain. This is because the herniated disc presses against nerves in the spine. This causes some signals to not get through properly, and the sensation won’t be normal.
- Weakness of the Legs: This is a serious symptom that you should seek medical attention if you have weakness in your legs or any other symptoms. The herniated disc may cause severe nerve compression, especially in the legs. If you feel this is you, it’s important to address it as soon as possible.
What are the L5 and S1 Pain Symptoms, and the L5/S1 Pain Pattern?
There is a common L5-S1 pain pattern when there is an injury to the L5 nerve root. The L5 nerve root, S1 or both can be affected. L5 pain is described as pain running from the OUTSIDE to the inner shin to the outer border of the feet. The S1 pain pattern is closer to classic sciatica, with pain running down the back of your leg and often into your toes. These are the most prevalent L5-S1 pain symptoms.
A herniated disc can present as L5/S1 symptoms.
- Leg shaking/spasms: These spasms can be confused with sciatica. The muscles tense up, causing spasms. A short course of muscle relaxants is the best treatment for this condition.
- Problems with the Bladder & Bowel: This alarming symptom should be treated as quickly as possible. The herniated disc L5/S causes nerves in the bladder and bowel that are responsible for their function to be compressed. Incontinence can also be called accidents. This is when the nerves that allow the bladder and bowel to do their job are compressed by the herniated disc at L5/S1. You should visit the emergency room if you can’t contact your doctor.
- Numbness in private areas (or “Saddle”): This is another symptom which requires immediate medical attention. This indicates that lower nerves are compressed and can’t function properly. You might have a permanent problem if this isn’t treated quickly. The next step should be to visit the emergency room.
Common Symptoms and Signs of L5-S1 Stemming
The symptoms of vertebral or disc pain between L5 and S1 may appear suddenly after an injury or slowly over time. A dull ache, or sharp pain, may be felt in the lower spine. Discogenic pain is often worsened when you sit too long, stand in one place, or do repetitive lifting and bending.
Radiculopathy symptoms, or sciatica may be caused by compression or inflammation of the L5/or S1 spinal neural nerve root.
- Pain is usually described as a sharp, shooting and/or severe feeling in the buttocks and/or toes.
- Numbness in the feet and/or toes
- Foot drop is a weakness in the foot or leg muscles.
You can also experience stabbing pains and aches that are specific to these (dermatomal)areas. Although these symptoms are usually limited to one leg, they can also affect both legs at times.
Cauda Equina syndrome may develop at L5-S1 when there is an injury to the cauda Equina nerves, which descend from your spinal cord. This syndrome is a medical emergency. It typically causes severe pain, weakness or numbness and/or tingling in one or both legs. It is possible to lose bladder control and/or bowel control. To preserve leg function and restore bladder and bowel function, the condition must be treated quickly.
Nonoperative Treatment
Although radiculopathy and low back pain are both common causes for disability, most patients feel relief from their symptoms regardless of how they are treated. A study15 of 208 patients suffering from radicular discomfort of an L5 or S1 origin found that 70 percent experienced significant relief in their leg pain within four weeks. It is advantageous to offer symptomatic treatment for patients who have symptoms of a herniated disc within six weeks.
Family physicians often play the role of educators, offering advice and suggestions on how to treat symptoms caused by a herniated or bulging disc. Patients with low back pain generally respond to conservative therapy. This includes exercise, limited bed rest and in some cases injections. The doctor must decide the best strategy for each patient and the goals. The physician should explain the patient’s condition in detail, including their likely natural history as well as possible treatments.
Bed rest can be used to reduce mechanical pain and intradiscal pressure when the patient is in a supine position. Although it is difficult to determine the optimal length of bed rest for patients suffering from herniated disc, most recommend a minimum of two to seven nights. Research suggests that a longer bed rest period of two to seven days is not better for patients with herniated discs 16. However, it has been shown that patients who stay in bed more than that amount of time are less likely to experience a worse outcome.
Aerobic exercise isn’t proven to be effective in relieving radicular discomfort. Many believe that strengthening abdominal and back muscles can reduce symptoms, weight loss, anxiety, depression, and anxiety. The patient and his family can learn how to massage and do exercises. First, isometric and extension exercises are done. After enough strength and pain relief has been achieved, flexion exercise can be permitted. Flexion exercises must be delayed as flexion movements place the largest load on the intervertebral disc.