A cervical herniated spine can lead to a range of different kinds of pain, or none at all. A range of pain may be felt in the neck and arm as well as in the hand. Sometimes, it radiates to these areas. There may be weakness in the hand or arm, or even numbness. The symptoms of a cervical herniated disc can be caused by injury or trauma to the neck. However, they are most often spontaneous.
The symptoms of cervical herniated disk pain and associated signs can usually be felt in one or both arms. Different symptoms may be experienced depending on the disc that has herniated or which nerve root has become pinched, inflamed, or both. Rarely, the symptoms of tingling, numbness, pain and/or weakness can extend to the arms or legs. However, it is possible for someone to lose control of their bladder or bowel.
Introduction
Together with intervertebral disks, the vertebral column is also known as the spine. It extends from the base of the skull to the coccyx. It also includes cervical, thoracic and lumbar regions. The spine plays several important roles in the human body. It protects the spinal cord and branches spinal nerves and provides structural support. It also allows for mobility and flexibility. The intervertebral Discs, cartilaginous structures located between adjacent vertebrae, support the spine and act as shock-absorbing pillows to the body’s axial loading.
The cervical spine is made up of seven vertebral bodies. These are C1 through C7. They run from the base and go all the way to the thoracic spinal spine. Unique properties distinguish C1 through C7 from C3 to 6’s typical cervical vertebrae. C3 to C6’s anatomy includes a vertebral head, a vertebral arch, and seven processes. The vertebral arch consists of the pedicles, which are bony processes that extend posteriorly from vertebral bodies, and the lamina. These are the bone segments that make up the majority of the arch. The pedicles, lamina, and the spinal canal are a ring that surrounds the spinal cord. The typical vertebra has seven processes. These include two superior and two inferior articular faces, one spinous process and two transverse processes which allow for the passage of vertebral vasculature.
The cervical region contains three unusual vertebrae. C1 (atlas), articulates with the base of the skull. It is unique in the fact that it does not have a body due fusion with the C2 vertebrae. The atlas can rotate around this pivot point. The C2 vertebra has a distinctive feature: an odontoid process (dens), which rises from its superior side and aligns with C1’s posterior arch. C7 is different from a typical cervical vertebra in two ways. First, the vertebral vein does not pass through the transverse foramina. Second, it contains along its spinous process. C7 is commonly called “vertebra prominens.”
There are seven cervical vertebrae. But there are eight pairs. They are numbered C1-C8. Each pair of cervical nerves comes from the spinal cord in the order of their respective vertebrae, with the exception of C8, which is inferior to the C7 vertebra. There are eight pairs of cervical nervous, numbered C1 through C8.
What Does the Meaning of ‘Herniated’ Mean?
The gel-like substance that lies in the center of the disks between vertebrae is found in their middle. The gel-like substance is contained within the disk’s outer layer, which is composed of fibrous cartilage. The gel can come out of the outer portion if it splits or tears. This is what happens when a disk becomes herniated. A herniated disk can also be called a “ruptured disc” or “slipped disk”. It’s similar to a jelly donut whose filling is squirted.
The Management of Cervical Herniated Disc Pain
The pain in the neck, arm and back caused by a cervical herniated disc can be temporary and last only for a few weeks. However, it could become chronic and last several months. It is not uncommon for the pain to recur or flare up during certain activities. The symptoms of neck or arm pain caused by a herniated disk usually disappear within 4 to 6 month, although the disc may still need to heal.
Most cases of cervical herniated spine pain can be treated with non-surgical methods. This includes over-the-counter pain medications, physical therapy to strengthen and stretch your neck, ice and heat packs, activity modifications to avoid painful movements, and/or surgery to relieve the pain. Sometimes, it may be necessary to administer oral steroids or an epidural.
How a Cervical Disk Herniates
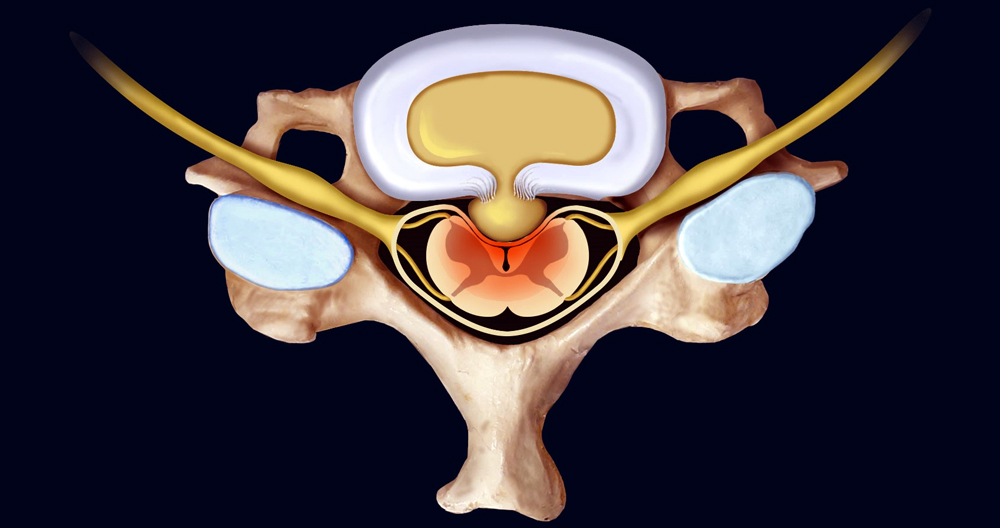
In the cervical spine, there are six intervertebral discs. Each cervical disc is placed between adjacent vertebrae (one higher than the other) to cushion vertebral bodies and distribute load from the neck. Two components make up a disc.
- Annulus fibrosus. Concentric collagen fibers make this outer layer strong enough to protect the soft inner layer. The annulus Fibrosus is responsible for absorbing shocks and distributing heavy loads to the spine.
- Nucleus pulposus. This gel-like interior consists of loose network fibrils suspended in mucoprotein jelly and protected within the annulus Fibrosus. The nucleus fibrosus offers additional flexibility and cushioning for movement.
A herniated disc is when part of the outer layer of the disc tears or the nucleus pulposus begins to leak into the tear. A herniated disk is most often accompanied by pain caused by the nucleus Pulsus, which contains inflammation proteins. Sometimes, the herniated disc can leak onto your spinal cord.
Risk Factors of a Cervical Herniated Disc
Age is a factor in the likelihood of developing a herniated or bulging disc. A cervical herniated disc most often develops between the ages 30, 50, according to some estimates. A majority of studies have shown that men are at greater risk for developing a cervical herniated disk. However, recent research suggests that women could be at increased risk.
In adults, cervical herniated discs occur at a rate between 0.5% to 2%. However, cervical herniated discs can often go undiagnosed. Estimates could differ by population.
The Seriousness of a Cervical Herniated Disc
Rarely, signs and symptoms of a cervical herniated spinal disc may become worse than they resolve on their own. Tinting, numbness, or weakness can occur in the arm if the cervical nerve root is not removed. Similar problems may occur if the cervical herniated disk compresses or inflames the spinal cord. These neurological disorders require immediate medical attention to stop them from getting worse or becoming permanent.
Etiology
An intervertebral Disc is a cartilaginous formation that includes three components: the inner nucleus of pulposus, the outer annulus fibrosus and the endplates that attach the discs with adjacent vertebrae. Disc herniations are when the nucleus of the nucleus protrudes through the annulus. This can be acutely or chronically. Chronic herniations happen when the intervertebral Disc becomes degenerated and discolored as part of the natural aging process. This can lead to symptoms of insidious, or gradual onset, that are less severe. Acute herniations are more common and result from trauma. This causes the nucleus pulposus to protrude through an annulus fibrosus defect. The injury can cause severe symptoms, which is more common than chronic herniations.
Epidemiology
Cervical disc herniation is more common in women than men, and it increases as we age. It’s most prevalent in those in the third to fifth decade of our lives. More than 60% of cases are females. The most common patients with this condition were those between the ages of 51 and 60.
Pathophysiology
The pathophysiology behind herniated disks is believed to involve a combination between mechanical compression of the nerve by bulging nucleus pulposus as well as a local increase of inflammatory cytokines. There are a variety of degrees of microvascular injury that can be caused when compressive forces exert pressure. This can include mild compression, which causes venous obstruction, and can lead to congestion and edema. Or, severe compression which can lead to arterial ischemia. The production of inflammatory cytokines can be triggered by nerve irritation or herniated disc material. This could include interleukin-1 and IL-6 as well as substance P, bradykinins, tumor necrosis-alpha and prostaglandins. The reproduction of symptoms may also be affected by stretching the nerve root. Because the cervical nerve travels along the neural foramen as it exits, it is susceptible to stretching. This arrangement could partially explain why certain patients feel pain relief when the arm is abducted. It presumably reduces the amount that the nerve experiences.
Posterolateral herniations tend to be more common, as the annulusfibrosus is thinner than the posterior longitudinal ligament and has less structural support. Radiculopathy in the dermatome can be caused by radiculopathy due the close proximity between the herniation site and the traversing cervical neural root. [10]
History and Physical
Cervical disc herniations typically occur between C5 and C6 vertebral bones. This can lead to symptoms at the C6 or C7 vertebral bodies, respectively. The history of these patients should include the following: the primary complaint, onset, aggravating factors, radicular symptom, and any previous treatments. Axial neck pain and ipsilateral arms pain are the most common subjective complaints.
When evaluating neck pain, it’s important to look out for signs that may indicate an underlying condition, such as inflammation, malignancy, infection, or other symptoms. These include:
- Fever and chills
- Night sweats
- Unexplained weight gain
- History of inflammatory disease, malignancy or systemic infection, including HIV, systemic infected, tuberculosis or drug abuse
- Pain that doesn’t stop
- Point tenderness is more important than a vertebral head
- Cervical lymphadenopathy
- Physical Examination
A clinician should assess the patient’s range of motion (ROM) as it can indicate the severity or degeneration of pain. For the evaluation of sensory disturbances, motor weakness, deep tendon reflex abnormalities and motor weakness, a detailed neurological examination is needed. You should pay attention to any signs of spinal cord dysfunction.
Common findings of single nerve lesion due to compression from a herniated cervical disc
- C2 Nerve: eye or ear discomfort, headache. History of rheumatoid and atlantoaxial instability
- C3, C4 nerve : vague neck and trapezius tenderness. Also muscle spasms
- C5 Nerve: Neck, shoulder, and scapula pain. Lateral arm paresthesia. Ear flexion and shoulder abduction are two of the most common motions. Also, weakness may be observed in forearm supination, external rotation, shoulder flexion and external rotation. Diminished reflex of the biceps.
- C6 Nerve: neck, shoulder and scapula pain. Paresthesia of the lateral wrist, lateral hand, and the lateral two-digits. The primary motions affected are wrist extension and elbow flexion. Also, weakness may be observed with external rotation, shoulder abduction and forearm pronation.
- C7 Nerve: Shoulder and neck pain. Paresthesia of the forearm and third fingers. Elbow extension and wrist flexion are the primary affected motions. Diminished reflexes in the triceps
- C8 Nerve: Shoulder and neck pain. Paresthesia of the medial arm, medial hand and medial two-digits. Tightness in thumb extension, handgrip, finger flexion and handgrip.
- T1 Nerve: Neck and shoulder pain. Paresthesia of the medial arm. Paresthesia that causes finger abduction or adduction weakness.
- The Spurling test and Hoffman tests are examples of provocative tests. Spurling test can help diagnose acute radiculopathy. This is done by extending the neck to the maximum extent and then rotating the head towards the affected side. This will cause radiculopathy symptoms to appear and narrow the neuroforamen. To determine whether there is spinal cord compression, myelopathy or not, the Hoffman test or Lhermitte Sign can be used. You can perform the Hoffman test by holding your long finger and moving the distal end downward. Positive signs are when the thumb can be flexed and adducted. Lhermitte signs are obtained by flexing the neck of the patient. This can cause an electric sensation that travels down the spine to the extremities.
Evaluation
A majority of cases involving acute spinal injury and herniation will heal within four weeks. Imaging is generally not recommended during this time, as the management of these cases won’t be altered. This period should only be used if there is a clinical suspicion of potentially severe pathology or neurological compromise. Further evaluation is required for patients who do not respond to conservative treatment within 4 to 6 weeks. Lab markers may also be recommended for patients who exhibit the above-mentioned red flag signs. These may include:
Lab values:
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP): These are inflammatory markers that should be obtained If a chronic inflammatory condition is suspected (rheumatoid arthritis, polymyalgia rheumatica, seronegative spondyloarthropathy). They can also prove to be useful if there is a possibility of an infectious condition.
- Complete blood count (CBC), with differential: Used in situations where infection or malignancy may be suspected.
- X-rays: This is the most common test and one that can be done in most outpatient and clinic offices. Three views (AP and lateral) help to determine the overall alignment of the spine. They also check for any degenerative, or spondylotic, changes. These views can also be supplemented with lateral extension and flexion views to check for instability. Imaging that shows an acute fracture may require additional investigation with a magnetic resonance imaging scan (MRI) or computed tomogram (CT). An open mouth view (odontoid), may help in diagnosing atlantoaxial instability.
- CT Scan: This scan is the most sensitive to see the bony structures of your spine. It can detect calcified herniated disks and other insidious processes that could lead to bony loss or destruction. CT myelography may be an alternative for patients who are unable, or otherwise ineligible, to visualize a herniated distal disc.
- MRI: MRI is the best imaging modality to see a herniated disc. It also has the greatest ability to visualize soft-tissue structures, and the nerve as it exits from the foramen.
If a patient has equivocal symptoms and imaging findings, electrodiagnostic tests (Electromyography or nerve conduction study) may be an option. It can also rule out the existence of peripheral mononeuropathy. Electrodiagnostic testing is sensitive enough to detect cervical radiculopathy between 50% and 71%.
Management / Treatment
- Conservative Treatments: Most acute cervical radiculopathies due to a herniated spinal disc are treated with non-surgical treatment as the majority (75 to 90%) will improve. These are some of the options that may be considered:
- Collar Immobilization: A brief course (approximately 1 week) of collar immobilization can be helpful during acute neck pain.
- Traction: May help reduce the radicular symptoms that are associated with disc herniations. Theoretically traction would increase the neuroforamen and reduce the stress on the affected nervous, which would in turn lead to improvement in symptoms. This therapy involves placing 8 to 12 lbs. of traction at an angle approximately 24 degrees of neck flexion over a 15- to 20 minute period.
- Pharmacotherapy: There is no evidence that non-steroidal immuno-inflammatories (NSAIDs)are effective in treating cervical radiculopathy. These drugs are often used and can prove to be beneficial for some patients. Although the analgesic effect of COX-1 inhibitors is not affected by COX-2 inhibitors, COX-2 inhibitors may have a lower gastrointestinal toxicity. For severe pain that lasts for a brief period, doctors can recommend prednisone as a steroidal antiinflammatory medication. A common regimen involves prednisone 60 to80 mg/day over five days. The dose can then be slowly reduced over the 5 m- to 14 days. Prepackaged tapered Methylprednisolone doses that range from 24 mg to zero mg are another option. This tapered regimen can be used for up to 7 days. Opioid drugs are generally avoided since there isn’t enough evidence to support their use. They also have a higher risk of side effects. For a brief time, a muscle relaxant may be considered if you have muscle spasms. A dose of 5mg taken orally three times per day is an option. For neuropathic pain treatment, antidepressants (amitriptyline or pregabalin), and mild analgesics (gabapentin or pregabalin) can be used.
- Physical Therapy: Commonly, after a short rest and immobilization. Some of the options include strengthening exercises, range-of-motion exercises, heat, ultrasound, or electrical stimulation therapy. No evidence has been presented to prove their effectiveness over placebo despite their regular use. There is no evidence of harm and their use is encouraged in the absence of myelopathy.
- Cervical Manipulation: There are limited studies that suggest cervical manipulation might provide some short-term relief from neck pain and cervicogenic migraines. The most common complications from manipulation include worsening of radiculopathy or myelopathy as well as spinal cord injury and vertebral arterial injury. These complications are common in 5-10% of 10 million manipulations.
- Interventional Treatments: Spinal steroid injections can be used as an alternative to surgery. Perineural injections are available with pathological confirmation via MRI. These procedures should be performed under radiologic guidance. The use of neuromodulation techniques to treat radicular pain secondary disc herniations has increased in recent years. These techniques mainly consist of a spinal cord stimulation device as well as an intrathecal pump. These devices provide minimally invasive, effective treatment options for patients not able to undergo surgical intervention.
- Surgical Treatments: There are many options based on pathology. Because it removes the pathology and prevents future neural compression, the anterior cervical discectomy is the gold standard. An option for patients with anterolateral sheniations is a posterior laminoforaminotomy. The new treatment modality of total disc replacement remains controversial.
Different Diagnosis
These are some examples of differential diagnoses
- Brachial Plexus Injury
- Degenerative cervical Spondylosis
- Muscle strain
- Parsonage-Turner syndrome
- Peripheral nerve entrapment
- Tendinopathies in the shoulder
Prognosis
A herniated disc can cause pain, restricted movement, and radiculopathy. In most cases, the symptoms subside within six weeks. This is due enzymatic resorption of extruded disc material. It is possible that the extruded disc material may be less hydrated or have a greater effect on the local edema. This could lead to pain reduction and function restoration.
About one third of patients will have persistent symptoms even after non-operative intervention. If symptoms last more than six months, it’s less likely that the condition will improve without surgical intervention.
Complications
Most complications from steroid injections will be mild and can occur in between 3% and 35% of cases. There are also more serious complications.
- Nerve injury
- Infection
- Hematoma of the epidural.
- Epidural abscess
- Spinal cord injury
These complications may occur after a surgery:
- Infection
- Recurrent laryngeal and superior laryngeal injuries.
- Esophageal injury
- Vertebral or carotid injuries
- Dysphagia
- Horner syndrome
- Pseudoarthrosis
- Adjacent segment degeneration