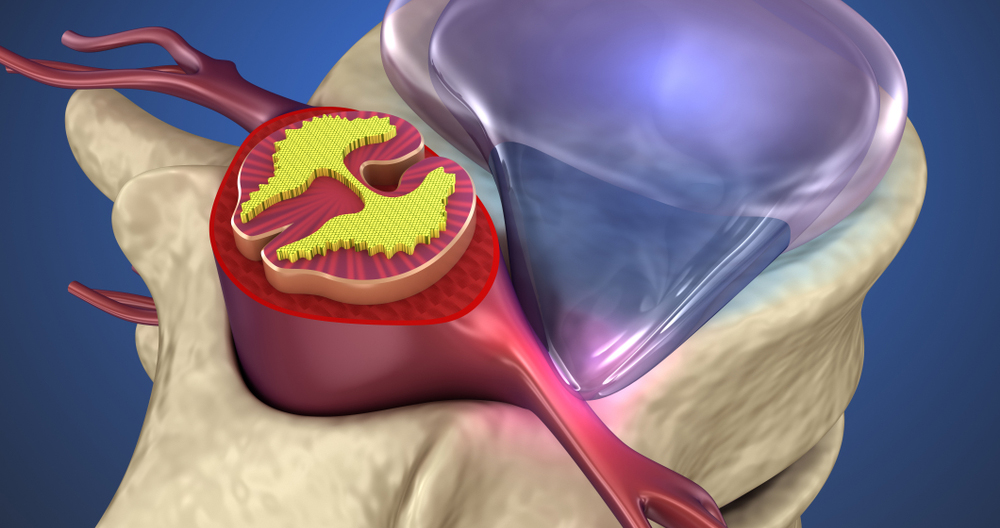
Anatomy of the spine and the specific parts that are involved in a herniated disc is useful to help you understand how it happens.
Anatomy of the Spine and its Function
The intervertebral cushions are the shock absorbers that cushion each vertebra of your spine. There is one disc between each vertebra. The discs have a hard outer ring of fibers called an annulus and a soft center, called the nucleus. The annulus is the outermost layer of a disc and the most powerful area. The annulus is a strong ligament connecting each vertebra. The main shock absorber is the disc’s nucleus.
A herniated or damaged disc is when the disc’s outer fibers (the annulus)become damaged and the nucleus of the nucleus pulposus soft material bursts beyond its normal space. The nucleus-pulsus material can push into a spinal canal if the annulus ruptures near the spine canal.
Low back problems can be caused by many factors. The terms ruptured and slipped disc are more often used in the last 20 years. People assume that every backache is caused by a ruptured or slipped disc. It is very rare to have a herniated nucleus pustulus (the medical term for this problem). Most back problems are not caused by a herniated or bulging disc.
Herniated Disc Causes
However, herniated discs can also occur in children. A true herniated disc is usually found in middle-aged to young adults. As we age, there are less chances of developing a true herniated disc in older people due to the degenerative changes occurring in the spine.
Too much pressure can cause discs rupture. Falling from a ladder, or landing in a sitting posture can all cause significant force to the spine. If the force applied is sufficiently strong, a vertebra may fracture or break, or a disc can burst. Bending over puts a lot of pressure on the discs between vertebrae. A disc may burst if you bend over and lift too much.
The disc can also break if it is subject to a very small amount of force. This is typically due to weakening in the annulus fibers caused by repeated, cumulative injuries. At some point, the annulus may weaken and you may lift or bend too far to cause too much pressure. You are doing something you would never have done five years ago that could cause a problem for the disc. Such is the aging process of the spine.
A herniated spinal disc can cause problems in two ways. First, the material that has exploded into the spine canal from the Nucleus Pulposus can put pressure on nerves. Evidence also shows that the chemical irritation to the nerve roots may be caused by the material from the nucleus Pulposus. Both the chemical irritation as well as the pressure placed on the nerve root can cause problems with the nerve root’s functionality. Combining both of these can result in pain, weakness, and/or complete numbness around the nerve root.
The Herniated Disc Symptoms
Sometimes, the symptoms of a herniated disc are not accompanied by back pain. A herniated spine is caused by nerve pressure and irritation. But many people have back pain due to other problems that may have occurred when the disc burst. Symptoms of a herniated spine include:
- It is possible to feel pain in one or both legs.
- Numbness and tingling in the one or both legs
- Muscle weakness in certain muscle groups of one or both legs
- Loss of reflexes in one leg or both
Depending on which nerve has been affected in the spine, these symptoms will vary in their location. Your doctor will determine where the symptoms are located. Your doctor can determine the likely location of disc rupture by knowing exactly where the pain is felt.
Herniated Disc Diagnosis
To diagnose a herniated Nucleus Pulmonosus, your doctor will need to have a full history and an examination. Your doctor will want to know the following:
- Are you suffering from an injury?
- Where is the pain,
- Is it numbness or weakness? Where?
- Do you have any weaknesses? Where?
- Have you ever had this or another similar problem before?
- Do you remember any recent weight loss or fevers?
Your doctor will want to know if there are any problems with your bladder or bowel movements. This is to ensure there is no pressure in the nerves running to the bladder and bowels. If this happens, it may be an emergency situation that requires immediate surgery. Your doctor may suggest X Rays of the lower back. A regular X Ray will not reveal a herniated spine, but it will give your doctor an idea how worn and tear the spine is and could help you to find other causes.
MRI scanning is the most widely used diagnostic test for a herniated spinal cord. This test is painless. It’s very accurate. There are no side effects as far we know. It has almost entirely replaced other tests such as the myelogram or CAT scan as the best (after Xrays) test to perform if there’s a possibility of a herniated spine.
Sometimes, an MRI is not enough to tell the whole story. It is possible to order additional tests. It may be necessary to have a myelogram combined with a scan of the CAT. Additional, more specialized tests might be needed if the pain isn’t coming from a herniated or bulging disc. A damaged nerve can also be confirmed by electrical tests such as the EMG, SSP and others. These tests can be required before the surgeon makes a decision to perform surgery.
Herniated Disc Treatment
The fact that your disc has herniated doesn’t necessarily mean that you will need surgery. A herniated spine will likely not need surgery in most cases. It all depends on what symptoms you have. It is also dependent on whether your symptoms are getting worse, or improving. Your doctor may suggest surgery if your symptoms are becoming more severe. If your doctor notices that the symptoms are improving, he might suggest waiting to see how they go. Many times, people who first have issues due to a herniated spine find that they resolve in a matter of weeks or months.
Conservative Treatment
Observation
There may not be any need for treatment, other than to monitor and ensure that the problem does NOT get worse. If the pain is not unbearable and there are no signs of weakness or numbness, you may be able to wait and watch.
Rest
If the pain is very severe, you might need to rest for a couple of days and slow down your activity. You can start to move after several days. Start walking slowly and increase your distance each day.
Pain Medications
You can use different methods depending on the severity of your pain to control it with medication. Some medications, including Tylenol or ibuprofen (over-the-counter pain medication), may help to relieve your pain. You should always follow the directions. Do not take more than you are instructed.
If you are still experiencing pain, your doctor may prescribe stronger painkillers – either narcotics or non-narcotics. Narcotic pain medicines can be addictive. Non-narcotic pain relief medications are less addictive and more effective than narcotics. Most doctors do not recommend narcotics being prescribed for longer than a few days, or even weeks.
Epidural Steroid Injection (ESI)
The ESI is typically reserved for those with more severe pain, such as a herniated or ruptured disc. Unless your pain is severe, surgery is often an option. The ESI will only reduce the pain of a herniated spine in approximately half of the cases it is used.
Surgical Treatment
Laminectomy & Discectomy
The laminotomy and discectomy are the two most commonly used methods to treat herniated discs with surgery. Laminotomy refers to making an opening in the lamina and discectomy refers to “removing the disc”.
This procedure involves making an incision along the center of your back and removing the herniated area. After the incision through the skin is made, the muscles must be moved to the sides so that the surgeon can inspect the back of each vertebrae. In order to determine the correct vertebra, it may be necessary for the surgeon to take X Rays.
A small opening will be made between the two vertebrae containing the damaged disc. This allows the surgeon into the spinal channel. Because of this, the term “laminotomy” (make an opening within the lamina), refers to the fact the surgeon must usually remove a small amount from the lamina bone. This is so that you can see into your spinal canal and make it easier to work.
After that, the surgeon moves nerve roots out of the way to reveal the intervertebral disc. The surgeon will then find the disc material which has burst into a spinal canal and remove it. This will relieve any pressure and irritation on nerves. He then removes any remaining nucleus pulposus from the disc with small instruments. This is done to stop any disc material from herniating again after the operation. After the procedure is finished, the muscles around the spine and back will be restored to their original positions. The incisions are closed with sutures and metal staples.
Microdiscectomy
Recent advances in tools have allowed spinal surgeons to perform discectomy and laminotomy with greater precision. The procedure is basically the same as for removing a ruptured disc, however it requires a smaller cut. This procedure has a few advantages over the traditional method. It causes less damage and pain to the spine. You might also recover quicker. A surgeon uses an operating microscope in order to see through the tiny incision. A tiny incision is made in your back at the spot where the disc is herniated. It can be as small as 2 inches. Once the muscles have been moved and the vertebrae visible, the procedure can be finished with a microscope. The rest of the procedure follows the traditional method described above.
Endoscopic Discectomy
Special TV cameras have made many surgical procedures easier. The procedure is similar, however, smaller incisions (1/2 inch) are used to insert a special magnified television camera into the spine canal. This allows surgeons to view the disc material. These incisions are small enough to allow the camera and several other surgical instruments to be inserted. He does not look through a microscope. Instead, he looks at the TV screen while directing the specially designed instruments to remove disc material.
Now, it is routine to remove the cartilages and gallbladders from the knee with an arthroscope. The same method is being applied to spine surgery. Endoscopic discectomy might cause even less damage if microdiscectomy incisions are smaller. This surgical procedure continues to evolve and is not widely utilized. This procedure causes less damage to normal tissues around the spine. This can help you recover faster and avoid more complications.
There are consequences to delaying treatment
Most people will seek treatment to treat a herniated spine because they find the pain unbearable and need relief. While some may say that they have high pain tolerance so they wait for the problem’s resolution, others will not admit to having healed. If left untreated, a herniated spine can lead to other serious conditions that become chronic. To prevent this from becoming worse, it is important to see an Atlanta chiropractor immediately if you notice the issue.
A bulging disc can cause nerve damage and cut off nerve impulses. Incontinence, severe pains and partial paralysis may occur as the problem worsens. One example is saddle anesthesia. In this condition, the nerves are so compressed that sensations are lost in the inner thighs and back of the legs as well as the area around the neck. A herniated spine can often be treated non-invasively. However, if it is left untreated, the condition may become so severe that surgery is required.
Nerve damage
Nerve damage may result from untreated herniated vertebral columns discs.
Cauda Equina syndrome is one example. The cauda and equina are nerve roots located lower in the spinal column. They help control our bladder control and walking muscles. Cauda-equina syndrome can cause permanent paralysis. It can also cause paralysis in your ability and capacity to control your bladder or respond to sexual stimuli.
Even if the herniated disc doesn’t cause that condition, you may still experience nerve damage. Your herniated spine and the nerve it places pressure on could cause permanent numbness/tingling, especially in your hands and feet.