Slipped disc? The importance of MRI for detecting a herniated disc
A herniated disc, also known by the slipped disc or the degenerated disc, is a condition that can develop from a ruptured or old-age disc. It can also be caused by injury, accident, or degeneration. In this situation, the hard outer shell of the disc will pull a portion of the soft and cartilage from the inside of the disc. Herniated discs can sometimes be invisible, but severe pain can occur if the exact location is not obvious. A slipped disc usually heals itself, although it is possible to have therapy or surgery.
What are the Signs & Symptoms of a Broken Disc?
The spine is composed of a complex, intricate bony structure. Each vertebrae is protected from injury by a disc-shaped structure. Each disc is protected by an outer layer, called the annulus. The nucleus pulposus is a softer inner cartilage. The nucleus pulposus is pushed to the outside when the annulus breaks down due to injury, overuse, and aging.
This can cause nerve pressure to increase. This can cause a pain sensation that can become unbearable. If left untreated, it could lead to nerve and spine damage. A ruptured disc can cause symptoms that vary widely from person to person. The location of the herniated disc as well as the extent of herniation will be key factors. These symptoms can be affected by the individual’s ability to tolerate pain and their health.
- Lower back pain
- Radiating pain radiating from the back into the extremities
- Difficulty to move
- Numbness that is felt on the left or right side of your body.
- Extreme muscle weakness and uncharacteristic
- Frequent tingling and pain in the area affected
How is a Herniated Disc diagnosed?
A consultant Healthcare Professional will not recommend an MRI if a patient has any of these symptoms. Usually, an MRI scan is not required if chronic pain does not resolve after 6 weeks of conservative treatment, including stretching exercises, massages, pain relievers, and pain relief medication. Many patients with herniated discs in the neck and lower back recover well after non-surgical treatments. Some patients may require more extensive imaging or diagnostic testing to confirm.
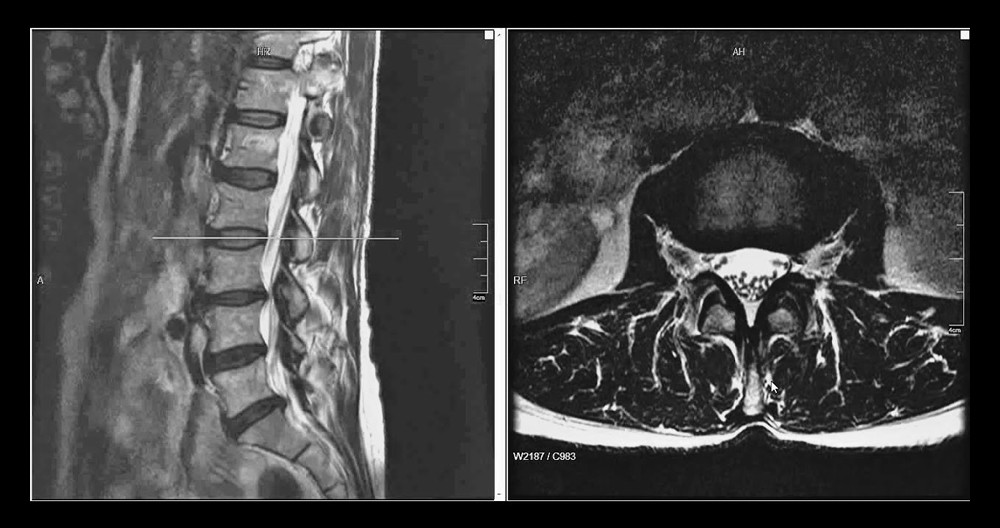
When surgery may be necessary, imaging tests are often used to confirm the presence or absence of a herniated disc. To check for a herniated disc in the neck, or any other part of the spine, a CT scan or MRI scan may also be ordered. MRI, among all imaging options, can provide the most accurate snapshot of the spine and aid in diagnosing a herniated disc. An MRI scan is able to pinpoint the exact location of the herniated disc and can also help in measuring the extent of the herniation. An MRI scan may also be helpful in improving the accuracy of surgeries and the time taken to recover.
Unusual pain on the spine is worth a visit to a physician in any case. Early detection and diagnosis can allow for the introduction of treatment interventions. This reduces the chance of developing irreversible complications.
Discussion
While MRI is useful for certain situations in lumbar pain, it cannot replace a comprehensive clinical assessment. The best way to manage radiologically matched clinical issues in lumbar back pain is to understand the limitations and advantages of MRI.
Multiple modalities can be used in spinal imaging. With better access to magnetic resonance imaging, and better quality imaging, primary care physicians will soon be exposed to nomenclature that is used by spinal specialists and neuroradiologists. This article clarifies the terminology used in lumbar spinal imaging and its clinical implications.
Clinical presentation
Spinal pathology patients often have a variety of symptoms. It is helpful to identify the three most common symptoms of spinal pathology – sciatica, lumbar pain, and claudication – as these can help you determine the cause. Although magnetic resonance imaging (MRI), is sensitive enough to detect spinal pathology, it can also discover a number of conditions that may have no clinical significance.
Lumbar back discomfort can be caused by many conditions, from muscular strain to facet joint arthropathy. The pain is usually located in the back, as the name implies. It can also be caused by localized damage to structures.
Sciatica on the other side has a different distribution of pain and is caused due to irritation of a nervous root. This could be due to either the compressive effects of an intervertebral disc herniation of a nerve root, or an underlying inflammatory process like infection causing acute pain distribution of a dermatome.
Claudication can be classified into one of two types: neurogenic, or vasogenic depending on the root cause. It often manifests as impaired mobility and dull, aching aches in the lower limbs. The most common form of neurogenic claudication, central vertebral stenosis, is a condition that causes neurogenic claudication. This is because it has a variable pattern while vascular claudication is more consistent.
In order to make a clinical diagnosis and differentiate benign from more serious conditions, such as spinal metastases or epidural abscesses, it is important to identify symptom chronicity. There are certain risk factors that may be present, including the patient’s age, medications history (eg. Steroid use and a pattern or stiffness could also be risk factors for ankylosing spondylitis or compression fractures. These would prompt further investigation using the appropriate serum tests and imaging.
Magnetic Resonance Imaging
Magnetic resonance imaging uses proton resonance technology for soft tissue cross-sectional representations. This allows the diagnostician, in comparison to other methods like computed tomography and lumbar (CT) myelograms to get more accurate and detailed images of the intervertebral area and its relation with the neural structures.
A systematic review of the available literature involving spinal MRI found MRI to be a highly sensitive and but less specific imaging modality for lumbar spinal conditions.For example, high sensitivity ranging between 89-100% for disc herniation have been described in previous studies.The lower specificity, 43-97% for disc herniation has been highlighted in previous literature and relates to the prevalence of asymptomatic disc degeneration and protrusions resulting in a large number of false positives.6 In a group of 57 patients with unilateral lower limb radiculopathy, only 30% of these patients had MRI findings of disc herniation and nerve root compression at the same level as the clinical prediction.Therefore, when reviewing the imaging, one must exert a degree of care when attributing the patient’s symptoms to the appearance of their lumbar spine.
An anatomy of the Lumbar Spine
The lumbar spinal column consists of five separate vertebrae that are separated by intervertebral discs. These discs are reinforced by multiple ligaments, paravertebral muscles, and multiple ligaments. The central vertebral channel houses the thecal sac that contains the conus and nerve roots. The nerve roots then exit from the spine via the intervertebral foraminal canal at oblique angles instead of right angles. This is also observed in the cervical spine. The clinician can identify the specific nerve root affected by the herniated disc by understanding this anatomical relationship.
The existing nerve root traverses the neural foramen. It is divided according to its relationship with the pedicle, zygapophysial joints in the axial or sagittal planes. In the axial plane the existing nerve roots traverse the subarticular recess between the central zone and the foraminal, extra-foraminal areas. To separate areas along the longitudinal axis, the following levels can be used: supra-pedicular/pedicular, disc and infra-pedicular.
In the annulus fibrosus concentric rings, intervertebral discs have a hydrated Nucleus Pulposus. The discs gradually dehydrate with age. A decrease in T2 signal is common in asymptomatic patients.
Spondylolisthesis
Spondylolisthesis can be defined as an abnormal alignment of the lumbar spinal column, in the form where a vertebra is slipping from its normal position relative to the inferior vertebra. This can lead to narrowing the lateral nerve foramen or the central spinal canal. Spondylolisthesis is also commonly associated with pars defects, lumbar spondylosis, and other conditions. Because of the chronic nature of the pain experienced by patients, as well as complex mechanical issues related to spinal malalignment, it is possible for conservative treatment to fail and surgery may be required. Anterolisthesis is found at the L4-5 Level, which results in severe central canal stenosis and neural foraminal stasis. There is also associated nerve impingement
MRI can be used to diagnose and assess the severity or potential causes of neural foramen or central spinal canal stenosis. The static nature of MRI imaging is acquired while the patient lies down. This makes it difficult to maintain stability at the affected levels. For the assessment of any exaggerated spine malalignment, spinal surgeons have used dynamic plain X Rays for the lumbar spine. This implies nerve impingement or further stenosis. A future addition to dynamic MRI spine imaging studies could be a better option.
Commonly Asked Questions
Can an MRI be used to diagnose a herniated disc?
Some physicians still recommend CT scanning or X-rays. Herniated disc MRI is still the best diagnostic procedure, as it provides the most accurate imaging for the condition and does away with unnecessary radiation. However, MRI scanning can be delayed by a clinician if the patient has had 6 weeks of worsening or persistent symptoms. The patient may then be offered a combination or conservative management strategies to ease the symptoms and improve their condition. Although most people are able to recover without any major surgery, there will be some who need further treatment. This is when MRIs are often prescribed.
Is a ruptured disc equal to a herniated disc?
A herniated or ruptured disc is the same spinal condition. It will show more protrusions than a bulging disc. Scans will also reveal that the cartilage usually held within the spine is leaking out to the outer, more rigid cartilage. Because it is likely to press on nerves it causes more severe pain than a bulging disc.
What happens to a herniated disc if it isn’t treated?
A herniated disc can worsen if it isn’t treated immediately. Most cases of slipped discs can be managed without surgery. A non-surgical treatment for a herniated disc can include relaxation, physical therapy and the use of painkillers. Neglecting to treat the condition can result in permanent nerve damage. This condition can cause loss of bladder control and bowel control. It can also lead to sensation loss around the thighs or rectum.
Can MRI detect herniated discs?
A MRI scan is used to confirm a herniated-disc diagnosis. It can pinpoint the area of the spine showing herniation. This allows for better management of treatment, which may in some cases involve surgery.
What causes herniated discs?
Multiple causes can lead to a herniated disc. Disc herniation can also be caused by accidents and normal wear and tear due to aging. These are just a few of the possible causes.
- Poor posture
- The incorrect positioning of heavy objects can often cause unnecessary strain to the back.
- Overweight or obese can place unnecessary pressure on the spine.
- Regular physical activity is not enough
Summary
Better treatment can be achieved for patients with radiologically matched clinical issues if there is a better understanding of the limitations and advantages of MRI in evaluating lumbar spine pain.