Magnetic Resonance Imaging (also known as MRI), is one the most important innovations in modern medicine. The MRI allows surgeons the ability to diagnose and accurately assess conditions that could have a life-threatening outcome. MRIs are helpful in many aspects, including the examination of spine conditions.
MRI scans for herniated discs can help to locate the exact problem and determine its severity. Patients with symptoms of herniated discs will often be advised to have an MRI done before they complain.
MRI scans are non-invasive tests that can detect herniated or bulging discs, and annular tears. Doctors can detect herniated spine discs with over 95% accuracy using MRI scans. CT scans do not use harmful x-rays. They are less accurate because the soft tissue structural changes that can be seen in a herniated spine are obscured by factors. CT scans can be used to assess spinal alignment, bony issues and other conditions such as those associated with spine fractures. MRI scans are highly accurate in displaying the spine discs and any issues surrounding them such as inflammation or degeneration. MRI is widely used to assess disc injuries.
What is a Herniated Disc MRI, and When Do You Need It?
MRI scans are used frequently to diagnose and monitor herniated spines. One of their most popular uses is to locate the herniated disc(s), and measure nerve compression. If your doctor finds a herniated or bulging disc on the MRI, they may recommend further tests to better evaluate the condition. MRIs are helpful in diagnosing bulging discs in neck and back and herniated disks.
What Your Doctor Might Do
Once your doctor has ordered your MRI, the technician will place you inside a tube-like device. The device rotates a magnetic field around the patient, changing the amount of excitation of hydrogen atoms within the tissues. Once the magnetic field has been removed the hydrogen atoms are in their normal resonance and release a small amount of energy. This energy can be detected by the scanner to create the image, known as an MRI scan.
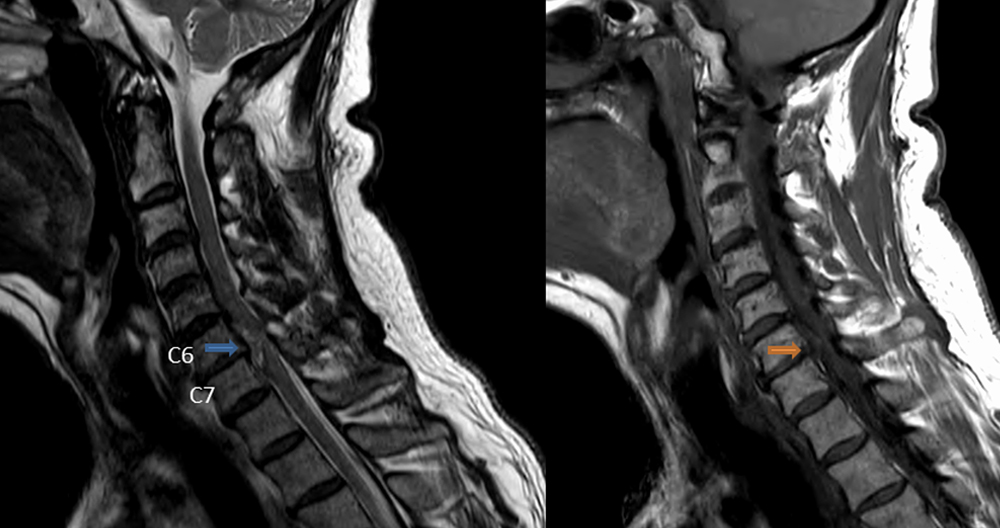
The generated MRI scan image shows anatomy. This is done by distinguishing between tissues that contain a lot (such as discs or cerebrospinal fluid) and tissues that contain very little water (such bone, cartilage, skin, and nerve root). Once the image has been generated, your doctor will examine it to identify any anomalies. MRI scans are sensitive to detect disc injuries, such as a bulging disc or bulging disc.
MRI protocol
Patients with nerve compression symptoms are easy to diagnose using MRI. We use the sagittal T1W/T2W-images to determine the level of suspected pathology. Because you are also trying to image the prevertebral soft tissues, don’t use a saturation band or a rectangular view (RFOV). An aneurysm within the abdominal organs is a sign of low back pain. Sometimes, it can be difficult for clinicians to differentiate neurogenic from arterial claudication. The frequency-encoding must be done in the AP-direction.
These have several benefits:
- The frequency-encoded direction provides the best resolution.
- We need the highest resolution possible in the AP-direction for the detection of small herniations as well as the delineation and marking of nerve roots.
- You can get breathing artifacts if you have the phase encoding set in the AP-direction. Some use a saturation or the RFOV to achieve this effect.
- These problems can be avoided by frequency-encoding within the AP direction.
- Frequency encoders in the feet head direction can lead to poor delineation. This is due to chemical shift artifacts, when the fat of the vertebral bodies meets the water in the disc.
- Another reason to use a feet head phase encoding or an AP frequency encryption is because of this.
It is better to have continuous slices of the same angulation paralleling the level at which nerve compression is suspected. This gives you the opportunity to track the nerve involved along the four possible levels of compression. Multiple levels, with different angles like the one to the right, will make it difficult for you to follow the entire nerve tract.
How to read an MRI for a Herniated Disc
The interpretation of an MRI scanning depends on many factors. Like many other diagnostic tests such as MRI scans, the challenge with MRI scan results is that the “disorder”, which is shown on the MRI scanner, does not always indicate the cause of backaches.
Patients must have a basic understanding of how lumbar MRI scans are done to determine if there is a herniated or damaged disc. These discs are usually in constant motion which can cause wear and tear. The annular tear occurs when the disc’s outer layer is damaged. This causes the inner nucleus jelly to leak into the spinal canal and form a hernia. This hernia can often be seen as a contrast spot on an MRI.
As a rule of thumb, MRI scans are interpreted according to the physiological symptoms that the patient experiences. An herniated disc may not present symptoms on its own. However, there are many people who suffer from undiagnosed back conditions.
The herniated disc can become protruding or bulging and cause severe pains. When the herniated disc is inflamed along its posterior annular tear, back pain can occur. The pain signals travel via the sinuvertebral nerve located along the margin of the Annulus Fibrosus. The somatic afferent pain fibers located along the posterior annulus fibrosus wall are called the primary sensory cortex. They project pain signals to the region of the brain that has highly localized pain.
Evaluation of MRI Scans Results
First, MRI scan results can be misleading. Unlike other diagnostic tests, the “abnormality”, as it is called, might not be the actual cause of your back pain. Numerous clinical studies show that about 30% of those in their thirties to forties have a lumbar Disc Herniation, even though they don’t experience any back pain.
A MRI scan cannot be interpreted alone. All information on an MRI must be correlated to the individual patient’s circumstances, including:
- Symptoms (such pain’s duration, location, severity and duration)
- Any neurological problems that were discovered during their physical examination
A key consideration when MRI scans will be performed is the timing. A patient with either of these conditions will require an MRI scan immediately.
- Incontinence in the bladder and bowel
- Nerve damage causes progressive weakness in the legs.
What is the best time to have an MRI to diagnose back problems
MRI scans can be recommended when patients complain of leg pain, a suspected lumbar disc herniation, or a combination thereof. The reason is that surgery to correct a lumbar disc herniation typically has few side effects and can lead to a quick return to normal function. A lumbar spinal fusion is the best option for patients suffering from lower back pain.
This type of spine surgery has a higher chance of complications (morbidity), and takes longer to heal. To determine if nonsurgical treatments (or conservative ones) will work, doctors recommend waiting three to six months after low back pain starts to subside. If the results of an MRI scanner are not going to impact a patient’s back pain treatment (and the patient will continue with nonsurgical treatments such as physical therapy and chiropractic treatments), then it is reasonable to wait to get an MRI.